Ricardo Echalar-Outbreak Epidemics in a Connected World
Good. Morning everyone. So. My. Presentation, is preparing for the next pandemic. But it's also. Trying. To get in front of the next pandemic learning, more about one health trying. To mitigate the threat. But. Ultimately. Recognizing. That with pandemics, it's not a matter of if it's a matter of when. And, that. Sort of leak you bet so I wanted to include that it's from it's. One from one of our projects. That we we do at USAID, called predict, which does a lot of wildlife sampling, to identify, viruses, circulating. In wildlife that may pose a threat to humans so, my name is Ricardo H alar I work with the US Agency for International Development we, used to sit right across the street now we're in the, the Global Health bureaus in Crystal City, my. Colleague. Kendra Chittenden and then Sarah page will. Be presenting, this afternoon, and. What. We do is on. Various. Degrees of. From. The. Prevention. Side to the detection side to the response of. Emerging. Threats, I. Oversee. Two global projects, one is called preparedness and response which, is working in 17 countries to develop multi sectoral, coordination. Platforms, that bring in human. Health animal, health environmental. Health sectors, together recognizing that one health is what will, drive our ability to better prepare and respond to these emerging threats and then, another. Project I work on it work, on is the. With. With the International. Federation of Red Cross and, Red Crescent Societies. Looking. At communities, because. That's where, these. Events start so how can we. Move. The equation to the left side get. To the very beginning and empower these communities, to do a better job of responding, and, and. Working, within, the communities and so, I just want to say thank you to Ashley for coordinating. All of these these talks I think this is incredibly exciting there's so many people in this room that could, be doing these talks themselves, so, thank you and and then, to Sabrina for curating. I think it's phenomenal that, we have an anthem apologist who is curating. Because we, know that, anthropology. And anthropologists, are needed, for outbreak response we saw that with Ebola we've seen that with influenza, and a. Recent article last week is talking, about in, the British Medical Journal on why, anthropologists. Are important for health so I recommend. That you look into that. So. What is a pandemic this, is a very basic. Definition, in, that a pandemic is a new disease that has spread globally in, order for it to spread it has to usually have efficient. And sustained human, human transmission meaning. That this disease can be spread between us. These. Two examples the 1918.
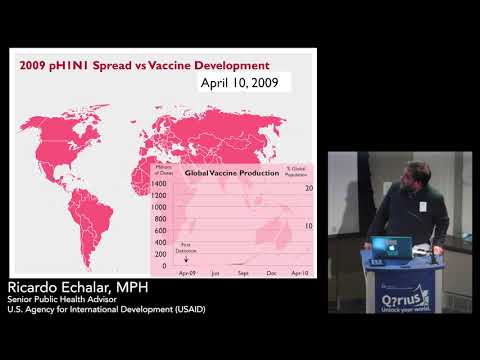
H1n1. Influenza. Pandemic, and hiv/aids, pandemic are probably, two that you are most. Familiar with I won't, go into specific, details. Of each disease because you'll get that today, but. These, are on the the, far end of spectrum in terms of both, high. Mortality, and. Economic. And social impact. As. You may know in 1918. The. Influenza. Pandemic. Resulted. In between, 50 to 100 million fatalities. That's. More than any wars. Combined. And, to. Put that in perspective if this. Scenario were to happen today which, was about 5% of the global population. That'd be between 200, and 400 million, deaths. Thankfully. A lot, has changed since, 1918. We have antivirals. We. Have vaccines and, we also have antibiotics, that deal with some of the secondary infections. With. Hiv/aids. Pandemic I put its. The, 1981. Figure here because of the, MMWR. Release. From 1981. That really. Brought. Attention, to this, this, outbreak at the time becoming, a pandemic. Which. Now about. 35, million people have died from this disease during. This time, but. With that said we, we, know that this disease. Predates. The 1981. Date. We. Have information. That. Samples. From Kinshasa in 1959-60. Have. Looking. Back at the them, we can see, the. HIV, virus. Or. HIV. There and then, probably origins, tracing back to the 1920s, so. Why, is, it that the. Disease suddenly, began to spread during, this time in the late 70s, early 80s and, not back in the 20s 30s 40s 50s 60s so. These are the think type of things that we're trying to identify and, trying. To get in front of before we, have the, next HIV, spreading. Globally. And something, in the, pandemic that you probably all very well. Remember, is the. 2009. H1n1, pandemic. That. Was also termed, the swine flu pandemic. So. You. Can see in this timeline, it started, first it in cases were detected, in Mexico, in April, 2009. The. Full, pandemic. Was, declared. By w-h-o in August and, by. September. You can see it's spreading. Incredibly. Around. The world and. One. Thing that I like, to mention, about influenza. Is that it really is sort of an equal-opportunity, virus. It impacts, both high resource and low resource countries. And. Impacts. Everywhere, so. After. One year of the initial detection, we. Had 2 billion people infected, that's, at, that time about a third of the global population. Though you. May then think about well what about vaccine, and that this is something that's important about pandemics, is that since it's a new virus, we did not have a vaccine, at the beginning of the outbreak. You. Can see. Going. Through the same timeline. Of. The, disease. That, we weren't able to capture the, the. Seed, strain or what we used to to, begin the production, of the vaccine until. Late. May and, then. From there. We, weren't. Able. To begin production until September, and. As. You can see six. Months we were at 7%. We. Could produce up to seven percent of the global population of, worth, of vaccine and then, one year. 17%. Now. Think about at one year or a 2 billion people had been infected so the vaccine in, reality was, not as an. Effective. Intervention. For. This disease, but. Vaccines. Are very important, public health interventions, so. There's an interesting. Initiative. Now called Coalition. For epidemic, Panda epidemic. Preparedness, innovations, and they're, looking, at about, 7 diseases, many of them are hemorrhagic fevers. To be able to capture. What what, may pose, the next threat and be. Able to scale-up vaccine, production for those threats.
Now. Influenza, is not one of those diseases because influenza, is, incredibly. Agile. Virus. That mutates all the time and as you can see with, our seasonal. Vaccine. Efforts sometimes they're. Effective, sometimes not as much. So. And Kendra. Will be talking about influenza. But that's. Something to consider as well. Though here. Are some of the pandemics, that we've had over the, last 100. Years. One, pandemic. On here that you may recognize, is cholera. Cholera, is a bacterial, pathogen, and. Has. Resulted in high economic, impact and. Disruption. Globally. And. Today. We. Still have lots of cholera, we're seeing large, outbreaks, in Yemen. In the Horn of Africa and, spreading across. Sub-saharan. Africa. But, what you can see here is that as, Sabrina. Was mentioning. These, pandemics, are of animal, origin okay. Except. For the, the colorado pandemic. The two that I mentioned the beginning h1n1, from, 1918, and hiv/aids, those, are on the far. End of the spectrum in terms that they had both high, economic impact, and. High. Mortality. We. Had two. Other. Influenza. Pandemics, in the 20th century with, h2n2, in. 1957. And then h3n2. In, 1968. Those. Were not as as, dire, as the 1918. Influenza and, then of course we had the h1n1. Pandemic. In. 2009. So, one thing to, note. Is that even. Though the 1918, is sort of the the, worst case scenario that we all think, about in terms of what we're planning it doesn't necessarily, mean that we'll. Have that scenario again like I mentioned a lot has changed. But. One thing that has changed that, we need to also consider from 1918, is that, within. 36, hours a person. Who is in hongkong can, be here in DC. Something. That wasn't, present. In 1918. Okay, so, we. Are living in a much more interconnected world, and because. Of that there are a lot of issues that we. Need to concern. Ourselves. With. Globally. Not just on a country level or a community level we are all connected. Okay. So. Why, should we prepare for the next pandemic and this. Is something that in. A lot of my work especially, in countries that are dealing with, tuberculosis. Malaria HIV. Things, that they are dealing with every day where morbidity, and mortality are, high it's. Hard for them to understand, why we need to, think about what's next. And when. You think about influenza. Pandemic, when there is a sudden surge of people seeking, care and treatment. Facilities, are, too. Full to be able to deal with those. Issues like HIV, TB. Malaria, where, do those people go, so. That's. Some, of the the. Considerations, that we have to think about and, knowing. That if, there, is even a mild to moderate, influenza. Pandemic. Availability. Of respirators. Of antivirals. Antibiotics. And a, lack of vaccine, will have an impact across. The health system globally. With. Ebola, we, actually saw that more, people probably, died from malaria than, Ebola itself, or. People. Were not able to get, proper. Prenatal. Or neonatal care. So. How can we address that how can we continue providing services. When, there is this new issue. In. Terms, of global, economic, loss there's. A study from the World Bank that says six trillion dollars, would, would. Be a loss. Of six trillion dollars would be the result of an severe, influenza pandemic, that's. Something that has repercussions for, many many years and something that's hard to recover from and finally. Social disruption. These. Diseases, are not just health issues, they go across the spectrum they. Impact. The economy, trade Commerce, tourism. Education. So, many times we see when there are these outbreaks schools. Have to close so what do you do then. Banking. Communications. You're. Thinking about these these, trade corridors, where you, know we depend, on, getting. Our, food from other country's well what happens when we cut that cut, those corridors off and we're. Not able to get the, the, foods that we rely on, and. Then, as we saw with Ebola another issue and I going. Back to the Anthropology side is trust, when. There is this type of large-scale, emergency who. Do we listen to. In Ebola, the three countries that were, post-conflict. States it was difficult for them to. Reconcile. Their, past in terms of their governments, and who, they were they're working with so they went back to who they knew community, leaders religious. Leaders, and. So we need to do a better job before.
The Next outbreak of. Knowing. Who should we talk to who should we listen to. And so, this goes back to one health as well so where do we begin. And. Recognizing. A Sabrina said, things. Have changed, over the years when so, I've been working in space for 15 years and when. I started I never thought about the animal health side I was, purely Public Health and. It's. Completely, changed my, way of thinking about how how this is done how we need, to approach Public, Health in general and recognizing. How interconnected we are between animals, and the environment, and. So. These these. Numbers are sort of what we are seeing, now and that's about, 75%, of these nearly emerging infectious diseases come. From animals, and that, includes the many diseases. That. Are part of this exhibit and then. About. 60%. Of known. Infectious, diseases were of, animal. Origin. So this is the one, health definition, that we have this, is something, that we work on closely, with us. CDC's. Office of, one health if you, need more information they have a great website I recommend, that you look there, and. The. One thing that I really, think you should take away from this is that. Human. Animal, and environmental. Health are all interconnected and. What. We're doing in, terms, of one health is we're, trying to achieve. The, optimal, health outcomes of all three okay. Though, three terms that I think you should also try to remember are spillover. Amplification. And spread. And if you want to read more there's a really great book by David quaint man called spillover. So what is spillover, spillover. Recognizing. That these emerging, diseases are coming from wildlife. Are. Able, to spread from. Wildlife to, humans. Or to. Livestock. Okay. So pigs. Poultry. And. Then. In, terms. Of amplification, it's, in the livestock section. That they are able to really, start to. Learn. And, be more adept, at then, being, able, to transmit, into humans, because we have more interactions, with livestock. Then we have our human to human transmission, usually. These are just small instances. Of human to human transmission we have these cluster cases, but, as I said viruses. Are incredible. In. That.
They Are always, learning they're always mutating. And they're, always trying to, continue. The spread. Though. In, humans, they can to continue to further amplify. And. Then. Spread in addition. Bill it becomes a, fully blown. Efficient. And sustained transmission. So. What we're trying to do is trying to get. All the way to the left, side of the. Of. The. Spillover amplification. And spread equation, trying, to see what, we can do before. These viruses can adequately. Spread, from wildlife, to, livestock and to to humans so, these. Are some of the opportunities in these pictures from, spillover, from animals. One. That. That. To, keep in consideration in, terms of Ebola is and, some. Of the other hemorrhagic fevers, that we've seen are. Bushmeat. Hunting so. People, who are. Tracking. And, hunting. And eating, bush meat may. Increase. Their risk of being, exposed to these these, viruses, another. Issue, our live animart, animal. Markets such as this, this. Market in Indonesia, with poultry, where. There. Is the threat of h5n1. Something. As. As. Everyday as pets. Our. Colleague. Casey Barton Baer Besh at CDC, one health. She. Has a whole. Work. On, backyard. Chickens. There's, a huge, growing, group. Of people in the United States who like, to have their, own poultry, in their backyard so what, happens is that increases, the risks of certain diseases that they are exposed to so. Greater. Socialization. Awareness, of what are these threats that you're dealing with with. These these animals and it's not just the threat from animals to humans you also have to think what threats, do we pose back to, the animals. Cats. And dogs get sick from the same viruses, that we have and thinking, on conservation, efforts, something, that I never thought about 15. Years ago when you're thinking about mountain, gorillas, that, are near extinction, is that they, are also susceptible, to. Flu viruses, and other viruses. That impact. Us and so we need to be careful with our interaction with them as well and, finally. Extractive. Industry and land use to change that's going back to the environment we see time and again whether, it's. Malaria. Whether, now, there's, further. Proof that the. West. Africa, Ebola outbreak, was because. Of these changing, environmental. Conditions, where. Wildlife. Are, living. In closer proximity. To. Livestock. Into humans. So, as we're changing because, of, logging. Or mining, we're. Changing, the whole ecosystem so, we need to think about how we can mitigate those risks. Nice. I. Don't. Know if this I hope. This will work so this is the NEPA example. From Bangladesh, that Sabrina, was talking about with those pots and it, when you're thinking about these these, palm trees it's, not much different than maple, syrup right you tap these trees you collect. This syrup, in, Bangladesh. They use it to drink it they, especially like it very fresh and the, bats like it even fresher so, they're, there on the trees they're, there saying thank you for tapping these these. Pots and. I don't. Think it's gonna work but. If. You can look it up this, is a fantastic, video, if you, like to see animals, that are urinating into, something, that people drink. So. So. Right away you see you see this animal interacting. With this pot and just, probably. Releases. This virus, into the pot that then the people then collect the next morning and they drink from so. Sabrina was saying there. Was a whole behavioral. Component, to this intervention. Behavior. Change is incredibly difficult just. Because you tell people, that there's. Probably virus in a pot doesn't. Mean that they're going to stop drinking from it, they're, they may not actually identify. With the risk so what are some of the interventions that they can do, that. Are easy and, culturally. Accepting, you can't just tell them to stop drinking it right, you can't tell people just, to stop smoking you can't tell people to just put on a seatbelt, you. Have to identify ways, that they can understand. What, are the benefits to them and also create. Incentives, that they, can they, can work with. So. Yeah look at look at this video if you can. Amplification, so. This is on the animal side where. Stocke who have been exposed to the wildlife viruses, are then kept, in close proximity to one another these, viruses, are then just going back and forth being, able to amplify between, these different species that, then have greater interactions, with humans so, we've see that in in, markets that have a mixing, of species, a.
Poultry. Of. Rodents. Of pigs. And then. That continues, to just allow. These viruses, to learn and adapt to be able to spread more efficiently to humans. Going. Back then. To, spread. 36. Hours is all it takes for these diseases to spread we saw that with. Influenza, we've seen that with stars we. Even saw that with Ebola now. Not all these diseases are. The. Same with. Ebola we, have the systems here in the United States generally. To be able to identify, and respond, to, these cases there may be a couple, of cases here and there but we have the ability to control. And and. Isolate. These patients, influenza. And respiratory illnesses are different, those. Those. Are harder to control because of mode of transmission being. In close proximity so, on who's coughing, or sneezing, is. Something. That we need to consider. And. Then. That has serious. Consequences. When. There is sort of this dis, event is that one of the first things a lot of countries. Or communities. Call, for is a, stop, and travel. And. So. It's. Probably. Not an effective intervention to completely stop travel it actually probably has more negative. Impacts as I was saying in terms of trade getting, commodities, to countries, and and. And. So. What. Have we done to, try to, to. Stop. The spread and move the equation to the left one. Of the issues that we are seeing, is that there needs to be better, farm, and market interventions. So, better. Biosafety. Biosecurity. Keeping. Species, separate from one another cleaning. Stalls, just. Regular. Waste management, things like that that can really have an impact in, in. Preventing. The the, viruses from spreading, from one another, and also. Than limiting. Interactions. Between animals. And humans, is important. At. The human, human interface, what really is important, is basic. Community, interventions. And. Infection. Prevention, control so in hospitals. Knowing. That there is a threat and and. Knowing. How, to properly. Clean and, keep, patients, separated, that may be infectious. Help. Stem, the spread. Of, spread. Further so we saw that with SARS, and we've seen that with MERS, identifying. These these, patients, quickly and isolating, them is incredibly, important. Dave this works, so. There was a movie. Probably. Released, about six. Seven years ago called, contagion, it's pretty sensational.
Poori. Is officer, dies in Minnesota. But. The. Last. Minute. Of the movie is probably the best minute of the movie because it. Shows sort of this spillover. Amplification. And the. Beginning, of the spread bats. Are not the. Enemy I. Bats. Contribute, a lot they are pollinators. And, so all, these animals that have these viruses. It's. Not their fault so we need to also understand. Intervention. Is not just to get rid of these animals, so that's something that. We're. To note. So what are we doing also, on terms of the preparedness, side so you. Probably know about the World Health Organization. They are the global body for for, human health. Technical. Norms and guidance and working with their member states to to. Issue. Policies. One, of the items that they've. That. Within. The World Health Organization, and member states agreed upon was something, called international, health regulations and, that was done in 2005, and went into action in 2007. Basically. As a result, of SARS how. Can we, create. Greater, accountability of. Countries, to be able to. Strengthen. Their health systems to identify these these diseases but also be. Transparent. And report these diseases to global community, acknowledging. That these diseases are not isolated. To countries and can spread, beyond. Borders. Within, the last couple of years they have something called the joint. External, evaluations. Which is an incredible, endeavor where, independent. External, experts come into country to be able to, assess. A country's, capacity. To prevent. Detect, and respond, to these threats looking, at wider health systems and it's doing this in a one health approach it's not just, human. Health on. The. Other side we have the world animal health organization, that's based in Paris and they also have these, codes, for aquatic and terrestrial, health. Basically. These are diseases that. Something. Like the USDA. On our side would have to report on when there is an avian influenza, outbreak which, there is quite, a lot in the United States how. Do they report it and who do they report it to and they, also have something similar to je that's specifically, for animal. Health it's called the performance of veterinary. Services to determine what are the capacities, in country of the animal health side. In. 2014. The, global, health security agenda, was, launched it's a, global. Multi, sectoral, multilateral. Partnership. That. Brings together both. Countries. And. Civil. Society, to a degree, together. To be able to strengthen, capacity, to better prevent. Detect, and respond, to these health threats. It's. Really trying to identify what are the, threats the country may have and how to strengthen their systems to deal with them. And. It's. Something that has, really we. Hope that will continue in, that recognizing. That. As. I said these diseases. Are, not. Isolated. Within, one country's borders but really do spread so it's not, just the health security of a certain country but on a global level. And, then. Finally, something. Just, like the, sepi, initiative. It's also a new. Initiative that's, pretty. Fascinating. And ambitious. It's called the global Byram project, and it's. It's, sort of thinking about. Where. We were in terms of the human genome project. Before, we. Could. Sequence the human genome. We. Didn't know much about how. We could apply that to medicine. Now and in diseases and so, trying to think and build off those efforts how can we do that on the viral. Side of things so, working, globally, over, ten year period to be able to identify the majority, of these unknown viruses, that are circulating that, can, infect, humans. And, it's. These. Are these are a couple things that the. Global health security agenda is really important it's strengthening, the systems now, to. Be able to deal with what's what's, happening in these countries now, but, also prepare, them for the future. The. Global. Viral project and sepi is trying, to even. Further, push, the. Envelope, trying to be able to get. The science down to understand, what are the things circulating, so that when something happens you, already have a foundation, to work from it. Will hopefully shorten, the amount of time to respond, to, be able to produce vaccine. Or other. Therapeutics. And. Reduce. Excess, mortality morbidity. So some take-home. Thoughts. In, the 21st century disease, emergence, is accelerating. Accelerating, and that's, driven by population. Growth and related. Impact on the environment there. Are a lot more people and a lot more. Interactions. Between people and these animals so. How can we deal with that that's why one health is important. Though. We have improved a lot since 1918. On. A global, scale we are still ill-prepared, to, deal with these emerging threats so. Global health security agenda, is, a good start and all these other global. Partnerships. Are a good start but we still need to do more and we. We, need to do more at the community.
Level, And empowering. Communities, to address, these issues. Our. Capacity, to deploy effective. Countermeasures. Is limited, by what we don't know about future threats okay. Too. Often what we do is fall back on what happened last time but, we need to change and think about what's going to happen next. And things. Like sepi and the global Byram project program, are our. Initiatives, that could help Lee, address. That and be able to know. More about what we don't know. Finally successful require changing, from a culture that is reactive, to one that is prepared and, this. Is, this. Is probably one of the things that are most hard it's hard for people to try to. To. Think about what, can you do now to prepare, for the next threat and not not, everyone, has to do that I mean there's simple things that people, can do to stem. Disease. Spread in general like hand washing and, non-pharmaceutical. Interventions such. As staying home when you're sick or, isolating. The sick from the, well. But. Trying, to I, think. I heard, a figure the other day that. 1. Million dollars, of. Preparedness. And Prevention, saves. From, 1 billion dollars, worth, of response and then 1 trillion dollars worth of recovery. So, it's, it's changing, that paradigm, and getting in front of it so. That's. My email address if you need to. Contact me I welcome, any. Questions. Or. You. Need direction. To anything I do recommend that you look into the global health security agenda. The, CDC one health page. Spillover. If you want a good book on the, material about David Clayman if you want more on the 1918, influence of Paul, Barry's the great influenza, and. This is a picture I took in Indonesia, and those, are all chickens that are going from market it, just thinking in Indonesia and kendry was there. They, have about 20, million chickens, coming, into Jakarta, a day and. It's. Probably one of the main epicenters, of h5n1, so, in a city. Like Jakarta. That's so densely populated the. Threat of a, virus, to be able to. Establish. Itself, in this population, and then amplify. And spread is something that is is, something that for. Us global health protection is public, health one health protection, practitioners, something, that we're trying to do a better job of preventing. So, that's, it thank you.
2018-09-08 23:40


