Tubes, Trachs, and Technology - Developmental Disabilities Update
I'm a pediatrician I work mainly on the hospital medicine service at UCSF Benioff Children's San Francisco and I also for the past three years have worked as the general pediatrician in our craniofacial center at the San Francisco campus serving as the only general pediatrician helping with those kids who have cleft lip, cleft palate, craniosynostosis, and other skull and facial differences. I have no financial disclosures I do want to disclose upfront that I'm not a gastroenterologist, a pulmonologist, or an otolaryngologist, or any other specific ologist. I'll be approaching everything from the perspective of a general pediatrician and how I approach these things and if anyone has other expertise so they want to share afterwards or correct me feel free, I am humble about all of this.
My goals are to review common technologies that your patients may use and maybe they're not your patients maybe they're just children in your lives. Provide some basic guidelines of what things can be done at home, in the office, and in the hospital and then I'll also outline some steps that primary care providers can take to provide some support to our children and their families. I want to start with an old definition which we don't really use anymore is this term technology-dependent children. When I started talking about this topic I was asked to give talks on technology-dependent children which Congress had defined probably not the right body to be defining technology-dependent children or children in general. But it was defined as children who need both a medical device to compensate for the loss of vital bodily function and substantial and ongoing nursing care to avert death or further disability, it's a pretty dramatic diagnosis.
But I also like to point out that this notion of requiring substantial and ongoing nursing care is maybe not as applicable in pediatrics since parents provide a lot of that. I should put that in quotations nursing care. We know that parents bear an incredible responsibility for children in general but especially kids who have medical complexity.
The preferred terms that are used now are children with special health care needs or children with medical complexity and I suspect that many others including Dr. Howtro yesterday touched on some of the definitions. I'm not going to go into too much detail just to remind us that these are kids who are increased risk of physical developmental, behavioral, or emotional conditions, and they require health care and related services beyond that they are required by children generally. It could be relatively minor things that are beyond the scope of what most children use or they could be pretty substantial things beyond the scope of what most children use. Some of the common technologies that I'm going to provide an overview of are enteral feeding tubes, long-term central venous access , and respiratory therapies.
My goal in doing this is to demystify it all a little bit such that those of you who are providers who are MDs and PSPAs, nurses, etc are more comfortable interacting with some of these technologies, and those of you who don't usually interact with medical technology just have a framework for how to think about them in what we do and in particular again revisiting the idea that parents actually do a lot of this care at home on their own. I'm going to start with just a little bit of the feeding tube alphabet because we throw around these terms quite a bit and say, "This patient has an NG or this patient has a G." Just to remind us that there are mainly three letters that come up and infer nasal or nose G for gastric, which refers to the stomach, and J for jejunal or the jejunum, which is the second part of the small intestine. The tubes are almost entirely labeled just by where they start and where they finish.
An NG tube a nasal gastric tube which is shown in the pink is going in through the nose and down into the stomach. An ND tube or a nasal duodenal tube is not very common. But is sometimes used for kids with bad reflux who have other small bowel issues that make it harder to advance the tube further but the more common if a patient doesn't have an NG is an NJ or a nasal jejunal tube and those are usually used when an NG tube is not tolerated either because kids throw them up or they have really bad reflux or gastroparesis and need to be fed past the stomach. Nasal inserted tubes are usually temporary tubes whereas G tubes also called gastrostomy tubes, are more long-term tubes that go through the skin and I'll show some images of this in a moment but again a G-tube is a more permanent option that goes through the skin.
You'll sometimes see the term PEG which stands for a percutaneously inserted or percutaneous endoscopic gastrostomy tube. In the hospital, the lingo between G-tube and PEG really just refers to whether it was placed by surgery from the outside in or by the GI service using an endoscope from the inside out and there's some subtlety of who's a better candidate for a G tube versus a PEG and then G tubes can be extended to GJ tubes so going directly into the stomach and through transpyloric to the jejunum and then there can also just be direct J tubes that never go into the stomach but go into the jejunum directly. Indications for home NG feeds in our kids some of the examples include kids who have inadequate caloric intake for a variety of reasons. It may be a neurologic condition, it may be a pain condition, it may be something else but kids who can't get adequate calories and also some of our kids have oral motor dysfunction so they can't successfully and safely get food from the front of their mouth to the back of their mouth so that they can swallow it. Then related to oral motor dysfunction is aspiration risk there are some patients who can move that food very well from the front to the back of their mouth. But when they tried to swallow they're at higher risk of swallowing and some of that food going into their lungs.
I always like to show just a little bit about NG tube placement and replacement. Since we do teach parents how to do this at home if any of you have seen small children with NG tubes, you know the first thing they want to do is pull them out. We definitely teach parents how to do this at home. When we're placing NG tubes we always want to start with a correct tube and what I mean by this is for those who work in health care settings you may notice that these feeding tubes are a smaller diameter and a softer yellow plastic than the suction tubes that we use for medical treatment of bowel obstruction or distention.
We measure the feeding tubes from the tip of the nose to the ear lobe to the xiphoid process, which is the bottom of the breastplate down to the umbilicus. We get the child in a position of comfort which I should point out this is not a position of comfort being held down on a table. We prefer to have the child sitting on the parent's lap with the parent hugging the child from behind and helping us then we lubricate the tube.
We insert the tube straight back and not up the nose looks like it points up but the opening is back and if we can have the child swallow and then after we place the NG tube, we confirm the placement make sure it's in the stomach before we use it for feeding. If you just think for a second you don't have to answer in the chat or anything but how do we confirm placement? Do we always take an x-ray? Do we listen for the stomach bubble? Do we do a pH assessment or just accept the fact that if the child is comfortable and not coughing it's probably okay? In the hospital, the answer is the most common method is the pH. We actually do a gastric aspirate check to make sure that we've got stomach acid.
That is obviously not an option if the child is on acid blockers because then we would not expect to get an acid aspirate. An x-ray can be used and then at home, we do teach parents to listen for the air bubbles, but we also encourage them to check for a gastric aspirate if the child is not significantly acid blocked because that's a good technique to use but recognition that we obviously can't do x-rays at home. When NG tubes get clogged, which happens all the time.
The preferred approach is to remove and replace because once An NG tube has been clogged once, it's likely to get clogged again. But if you have no additional tubes or if the tube is transpyloric or if it's a particularly difficult and challenging placement for other reasons, it can be unclogged. I find it crazy that Coca-Cola can dissolve the food material that clogs NG tubes or the debris in NG tubes but Coca-Cola actually does work. Then there are also clog-zapper products that are sold and then pancreatic enzymes that we use for supplementation can be dissolved in water, some of the formulations can be used to unclog the tubes.
But you want to be careful and double-check because some of them are not indicated to go through feeding tubes you will want to use the ones that can go through feeding tubes. Kids walking around with feeding tubes may use a pump. Some of them may only get feeds at home, but some of them may be carrying around a pump. This on the left is a hospital-style pump that we would not ask a child to tote around. But this child is wearing a backpack that has a feeding tube in it.
You can see off to the left this little tubing coming out of the backpack and into the child's gastrostomy tube. This is what a G-tube looks like from the outside. The reason there's a soda can tab under there is to remind us that the G-tube actually should not be tight against the stomach wall.
We want the G-tube to be loose enough that it can spin. That helps us ensure that the child is at low risk for pressure injuries. So if it's actually too snug against the skin, there's a risk of pressure injuries. I just like to remind people and when I check kids in the hospital, I usually makes sure that the G-tube spins nicely. Some complications that can happen with G tubes, infections can occur and you just want to distinguish that from granulation tissue. So if there's pasta and such, and rich erythema, that's more likely to be an infection.
Gram-positive infections are the most common and usually can feed through the infection. It's not usually an indication to remove the tube, but rather just treat with antibiotics usually systemically. Then if the G-tube gets dislodged, we want to immediately replace the tube and use a Foley catheter just to hold this space open if a tube isn't available because once these tubes come out the holes can close rather quickly. This is what the tubes look like when they're not in a person. This clear part here is the part that is going transpyloric or sorry, through the skin.
Everything above my cursor, the tubing and the housing up here would be outside the patient, and then inside the patient depending on what kind of tube it is, it either has a hard barrier to keep it from slipping out, or it has a balloon. I'll show you the balloon in a moment. This clear part is what's actually straddling the skin from the inside to the outside.
So this is what it looks like with a balloon. Again, these balloons are inside the stomach, anchored inside and they're filled with water, not air. Because like any balloon, if there were air, it would slowly dissipate and slip out so we fill it with water, doesn't have to be sterile water because if the balloon were to burst, it's just in the stomach as if we were drinking water.
So the balloon gets inflated just using a standard syringe and just for purpose of demystifying it I'm going to show this video and I hope the sound will work. But if not, I can narrate it a little bit, but this is just a parent changing a G-tube. Mommy is going to, okay. We're going to take the water
out and the pressure just pushes this out. Why are you taking the water out? Why are you taking that out? Are you changing it? Okay. Then you just pull it up. Maybe, ouch. Sorry. It's not ouch.
It's okay. Now put the new one in. Okay. It's okay.
Oh, can you empty this? Stretch fully. Is that inside his belly? Yeah, it is. Looks dirty. That one is and then you just want move to make sure. Is that inside his belly? You also want to give a little water. Again, that was just showing how a parent changes a G-tube and parents do this routinely at home.
We love to show people how to do it in the hospital or our residents and fellows don't always know how to do it, so it's a great little trick to show people. That was a high-level overview of enteral feeding tubes, I'm now going to talk briefly about long-term central venous access, which some of our patients have. The most common reasons our kids have central venous access is for parenteral nutrition, TPN, and some go home with IV therapies, and some kids dialysis, and then suddenly our kids who are on chemotherapy which they're not receiving at home, but so that they don't have to get accessed on a routine basis.
These are these kids who have need for extremely frequent access for dialysis and chemotherapy. Medium to long term, we use PICC, which stands for peripherally inserted central catheter, and long term is surgically tunneled or implanted catheter. PICCs, which are inserted by our PICC nurse in the hospital is, again as noted, peripherally inserted, so goes into one of the extremities, but it actually goes centrally into the SVCRA junction.
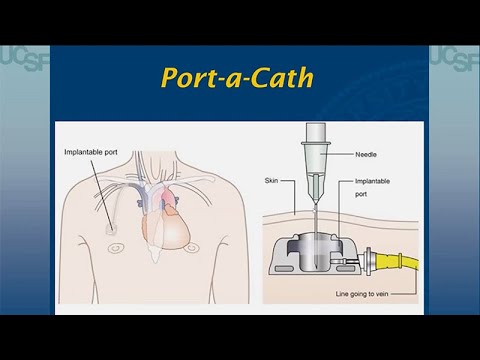
These can stay in for weeks to months. Broviacs, which are surgically implanted. This is what a broviac looks like from the outside and it's a common misconception looking at broviac that it goes directly into the heart from here. But in reality, what's happening with a broviac is it's just anchored beneath the skin, and then it actually usually gets tunneled up to the subclavian vein and then comes down into the SVC RA junction. By tunneling it under the skin, they both reduce the risk of infection and help stabilize it so it's harder to be accidentally removed. Then Port-a-caths are these catheters that are completely inserted below the skin so that there's no obvious external portion.
And these are accessed, similarly, they tunneled up under the skin to a central vein or to a vein leading to a central circulation and they're accessed using a needle from the outside and these are nice because there's minimal precautions required with respect to daily activities. Considerations of central line. Certainly, people can get superficial soft tissue infections around it. They can also get CLABSI, central line associated bloodstream infections.
At home, the management, there's usually actually very little care other than weekly dressing changes that parents can come into infusion centers for with younger children, but certainly, older kids may learn to do them themselves. Then these lines do have to be heparinized and depending on the line they're on a different schedule. Then I'll come to this at the end. But keeping in mind if lines get broken, dislodged, or otherwise non-functional is your emergency plan. In particular, for our patients on TPN, we may need to know if they're prone to hypoglycemia dehydration, that just gets it.
If the line stops working, does the parent have to come to the emergency department in the middle of the night or is it something for which the family can wait until morning to access? The third thing I wanted to talk about with regards to technology is respiratory therapies. We're going to talk briefly about oxygen therapy, cardiorespiratory monitoring, then a little bit about tracheostomies. Home oxygen. For the most part when patients use home oxygen and they are not getting these big giant canisters and cylinders delivered at home, for the most part what they use is concentrators, which are devices that basically concentrate room air.
Take the 21 percent FIO_2 of room air and concentrate it down to 100 percent oxygen. These concentrators are often in the home. They're not quite as portable as devices like this, so often our patients will have some type of portable oxygen canisters like for car trips and things like that. We'll make sure that they have access to oxygen cylinders. Oxygen is almost always through nasal cannula.
For our kids, it's usually 100 percent even kids who don't technically need it. Though, certainly, when you're on nasal cannula, even if you're on 100 percent FIO_2, you're getting a lot of inspired air. I think it's also important to note that kids on home oxygen are usually not on home monitors, and I'll talk about that in a moment. But in general, it's pretty unusual for us to send patients home on home monitors. The thinking being that if they really need to be monitored, then they may need a different setting.
Home monitors. When I started giving this talk, home monitors were not that common, now everyone can buy them on Amazon and COVID changed that landscape entirely so that everyone feels like they can have an apnea or pulse oximetry monitor. It's important to know that these are not all validated. Chris Bonafide at Children's Hospital of Philadelphia has probably done the most work on this and published. This is from four years ago rather just bought a couple of pulse oximetry, home baby monitors off Amazon, and found that they actually performed pretty poorly.
In the two that he tested relative to a hospital, monitor A detective hypoxemia but performed inconsistently. Monitor B never detected hypoxemia and also displayed falsely low pulse rates. Monitor B never went off but never actually found the problems. Really want to make sure that people are talking to their doctors or nurse practitioners or other healthcare providers about the appropriate monitors for them. Briefly about tracheostomies. We use them for airway anomalies.
Patients who require support of the upper airway tracheostomies can come in non-speaking and speaking versions, and they can have these humidifiers on the end. They can also have speaking valves on the end to help patients learn to speak with tracheostomies in. There are a lot of different kinds, and these are managed by pulmonary and otolaryngology together, and we actually have a trach vent clinic. Not everyone who has a tracheostomy requires connection to a ventilator, and not everyone who has a tracheostomy is 100 percent dependent if that tracheostomy gets clogged.
It's important to know if a patient with a tracheostomy actually can be hand ventilated, bag mask ventilated from above, and whether they can be intubated because some patients, if their trach should become occluded, can get bag valve mask ventilation through their mouth and some cannot, and can only be intubated endotracheally. Or cannot be intubated endotracheally either, can only be accessed through their tracheostomy stoma. It's really important to know as part of emergency plans for the kids.
I'll also mentioned, again, that parents do change tracheostomies at home. We teach people to always have a emergency phone available when you're changing a trach at home. I think for the purpose of time I'm not going to show the video of changing a tracheostomy because it's about four minutes or so. But it should be in the packet that you'll have access to. In general, Cincinnati Children's has really great patient education videos. If you just do a search for a Cincinnati Children's changing a tracheostomy video, you should find it, but the link is also in the handout that I submitted.
I just want to spend the last couple of minutes talking about some other things we can do in terms of disaster preparedness and emergency preparedness. The AAP actually puts out this example of an emergency information form for kids with special needs, and this is a place where, in addition to including basic demographic information, we document the child's information as well as what their diagnoses, past procedures, physical exams, etc are. What their medications are, what their other needs are.
The AAP has this form available for download on their website. I think it's very useful. I think we've all had patients who have these fantastic notebooks, these binders that parents have. Now what I'm seeing more and more is parents putting this information on a Google Doc or a Dropbox file or something.
People usually have them on their phones and just pull them up so they don't have to be carrying around these pieces of paper. I've even seen versions of it where people have a QR code where they can have it readily available either on their phone or on the child. One could envision that on the medic alert bracelet or something also just a QR code that takes you to Google Doc, or a Dropbox file, or something that has the appropriate information about the child. Then I'm sure that others have spoken on this as well. But I want to wind down by talking a little bit about some of the additional impact on these children that having medical technologies, feeding tubes, respiratory devices, central venous access, etc, has on children. Certainly, there's the emotional impact of prolonged hospital stays, kids also experience or at risk of experiencing low self-esteem.
There's also sometimes this sense of burden on their parents for some kids with medical complexity that I try to be aware of. Then the social impact. This one never really struck me until I read about it. This notion that kids who use medical technology may have very little alone time, where when they get into those teen years and they want their privacy, they always may have a nurse checking in on them, or a parent, or other caregiver checking in on them, and so that sense of having some privacy is actually very uncommon. You can imagine that kids who are connected to machines and alarms, all the more so if they're on a monitor rather that is alarming.
It could be quite distressful. Certainly, there are impacts on school related to what education classes they're in, and in particular, whether their school can accommodate the technology they use. Certainly some schools are very intimidated by medical devices. Then missing school appointments.
This is something that we found telemedicine visits have changed the dynamic and I'm sure you have also that parents find that they actually don't have to pull their kids out of school and we've even had some cases where schools created private spaces where the parents could show up midday, bring the kid to a private room in the school, and do the video visit from the school so the child had minimal lost at school. I think it's also important just to recognize that there's parent emotional strain related to the dependence of the child and the impact on family relationships, as well as this feeling that parents have no choice but to agree to technology dependency. Because they would never let their child die or suffer in other ways.
I think just keeping in mind that there can be an emotional impact on families, sleep disruption for monitors that need to go off for kids that are being fed every three hours or every four hours or something overnight. As well as the stresses of long hospitalizations and the economic burdens that go along with that. Fortunately, most of our technologies are covered by insurance or by CCS. But recognizing that missed work is usually not very well covered. The patients may have IHSS, or other support, but no doubt there are substantial additional economic burdens.
There can be disruptions to family, social life. Changes are lost in friendships. Some families avoid public outings.
Just a general need for respite and being aware of that families may need a break and that it is hard for family members, for caregivers to be aware of these technologies 24/7. They're on high alert all day and all night, and that can have a substantial impact on families. Then keeping in mind that when kids use feeding tubes, tracheostomies, etc, that it shifts the parent role into that of a, I probably shouldn't have used the nurse here. Just a medical care or health care giver and parents sometimes have to do painful or distressing procedures like replacing NG tubes and sometimes medical personnel are in the home, whereas normally that would not be typical in the home.
I'm going to whine down just by saying that I hope I've shown you that technology doesn't necessarily have to be complicated. Feeding tubes are actually quite straightforward and parents change them at home. Similarly, tracheostomies, maybe not quite so easy as you'll see when you watch the video that tracheostomy.
It's certainly quite a bit more complicated and high-risk than changing a feeding tube. But parents and caregivers who do this at home. I encourage you if you have the opportunity with one of your patients and you haven't seen a tracheostomy change to take that opportunity participate in the change. Primary care physicians, and again, apologies that should say primary care providers, are the first line of support for children with special health care needs. We encourage everyone to have an emergency plan. Again, always to be aware of the psychosocial needs of both our children and their parents as they navigate this journey together.
A couple of references that I have up there, and I will stop sharing because I'm right at 10:45 and I'm happy to take questions. Terrific talk. Thank you. Very practical. I hope that all the clinicians in our audience benefited from it and probably will play it over again and again. I have one quick question. What is the backup? We do have at most medical centers including UCSF, a fair number of patients who live in rural areas and commute to the medical center.
What if the trach comes out and they need some help at home? Yeah. It's a great question. Before families can leave the hospital with a child or dependent who has a tracheostomy. They have to be taught how to change the tracheostomy and they have to demonstrate their ability to do so. We do expect that as a skill if the tracheostomy should come out or should become clogged for some reason. We would advise people if they're ever concerned about the tracheostomy tube and can't get a new one in immediately, that they should call 911 immediately.
Don't hesitate, don't wait to see if you can find that backup tracheostomy. Just call 911, get emergency care there immediately. Most kids with tracheostomies can be bag valve mask ventilated.
If you have an ambu bag and we would make sure that families have this and a mask, they can be bag valve masked through their mouth. But we definitely tell parents, have a low threshold and that's why we actually teach them when they're changing the trach tube, that telephone right nearby, the cell phone or the landline just ready to call 911. To your point about them, families being in much more rural areas. It is quite a challenge.
I think we haven't quite gotten to the point of using telehealth in those truly emergency situations. Or someone could correct me if some of the more rural EMS services are now using telehealth for this. But it's certainly a good opportunity that one could get on FaceTime or a Zoom with a family and help coach them through it. If for some reason that family member can't remember the training they had or had concerns about it.
Thank you. Another question. Is there a list of recommended or more accurate over the counter devices like pulse ox devices, apnea monitors, etc? If there is, I don't have it. I can look into it and reach out to some of the people here.
But our perspective in the hospital is we always recommend that if someone needs a home monitor, then we want it to be through a DME company, through a health care company that provides it under a prescription. My general feeling is, I don't really like when families tell me that they buy home monitor is just because I think, again, it's a false sense of security. If we don't know how good those monitors are. I would have to look as to what's currently the recommended ones through a pulmonary and otolaryngology, but I've tended to stay out of that and rather just rely on what the DME companies can provide. A couple of questions about parents who can't be at home due to work. What's the insurance coverage for respite or home nursing? My understanding is that IHSS In home support services can provide respite care in many cases of often it's about eight hours a day.
Not a huge amount. IHSS is paying a family member to be at home during the day. Instead, basically compensating them for not being at their job that they would otherwise have an income source.
The family member is basically functioning in a nursing or other care provider role. Alternatively, some kids, we actually can try to arrange for home nursing depending on their care needs. It's more common in kids who have a ventilator dependence or have really significant medical needs beyond just one feeding tube or beyond a tracheostomy not connected to a ventilator, but kids who are dependent on tracheostomies and use ventilators may be able to get a home nurse. What we found over time though, is it becomes harder and harder to actually find the staff to go out there and provide that coverage. Our concern is less about getting the approval through the insurance or through CCS, and more about actually finding a reliable provider who can go out to the home and be that care provider.
A couple of questions about the impact on siblings who are not technology dependent and how do you connect parents who are being recommended these technologies so they can share what the experience is? There are a variety of support groups. Most of the specialties here at UCSF, are happy to connect people to different support groups for providers. Our Child Life Services and our Family Advisory Committee also have great resources.
For teens, the Child Life Services can sometimes connect teens to other teens who are in similar experiences. For younger siblings, they can help provide developmentally appropriate support. Then what I have found over time is that social media grows and grows, parents are finding more and more resources through Facebook groups or other online groups that are providing them with a tremendous amount of support. I would say that nobody knows better what the experience of living with a child with medical complexity is than the parents who do this on the front lines. They are often the best equipped and similar the siblings, people have found through some of these Facebook groups or other parent support groups, like support for families can connect siblings as well.
That can be tremendously helpful. I just want to point out a comment in the Q&A, which is about oral health. I think we don't have our dentists at this conference, but they would appreciate that we did a shout-out to remember oral health. Because sometimes there's a misconception that a person who isn't fed by mouth does not require the samedental care. Do keep that in mind. Absolutely. As long as they have as
long as they have teeth they are at risk for caries and aural abscesses and other complications. Definitely need dental care. I think it's also a good reminder that all of these kids also should have the same screenings as everyone else about things like tobacco exposure and other social determinants and making sure that they're getting the appropriate vitamins and such. Another from a clinician in rural California where we have power outages from time to time, brings up the question of should people with a child or family member on a ventilator support have a generator on hand? I think the short answer is yes. Is it covered by insurance? I don't know. Someone else might know,
but I do not know if the actual generators are covered by insurance. I know that the ventilators and the feeding pumps do have a certain battery life. But as we've learned, especially through wildfire season, that power can be out for much longer than one might originally anticipate. Having some a generator or other emergency power supply if you're not in an urban area, would be important.
The backup backup plan would be to take your child to the hospital if you lose power to call EMS or 911 and let them know that you have a child who depends upon a ventilator or if they have an equivalent device and needs an emergency power supply. Great talk. Thanks again. My pleasure. Thank you, Glenn. [MUSIC]
2022-08-09 12:52


