Technology to Improve Maternal Health: Plenary Presentation
Thank you so much to all our welcome speakers. We really appreciate your comments and your support of this initiative. And now I am very pleased to introduce our plenary speaker, Dr. Elizabeth Howell. Dr. Howell is a professor and chair of the Department of Obstetrics and Gynecology at the University of Pennsylvania. Her rich interests lie at the (indistinct) between quality of care and disparities in maternal and infant mortality and morbidity.
Dr. Howell has served on several expert committees, including the Institute for Medicine and the Joint Commission. She has co-chaired the Alliance for Innovation on Maternal Health Working Group on Reduction of Peripartum Racial Disparities and served on the New York City Maternal Mortality and Morbidity Steering Committee for the New York Department of Health. She was recently invited to the White House by Vice-President Harris to participate in a round table on black maternal health.
And now I invite Dr. Howell to give her talk on "The Maternal Crisis: How Did We Get Here and How Can Technology Help Us." Dr. Howell.
Thank you very much for the kind introduction, and it's really a pleasure to be here today. Next slide, please. I have nothing to disclose, and I will not be endorsing any technology product during this presentation. Next slide, please. So over the last decade, you've heard a great deal about the maternal healthcare crisis.
You know that our rates are higher than all other high-income countries in the United States and that there are significant racial and ethnic disparities. We've heard also over and over again that our hospitals, our health system, and our society is failing, are failing, excuse me, pregnant women and birthing people. Next slide, please. So the most recent estimate from the CDC puts our maternal mortality rate at 17.4 maternal deaths
per 100,000 live births. Next slide. That rate is actually higher than all other high-income countries, as I mentioned, but when you look and compare it to the World Health Organization's latest maternal mortality ranking, we would be ranked 55th. Next slide, please. And another slide, please. It's important to recognize the definitions, and I just wanted to briefly review that maternal mortality is a death of a pregnant woman, or somebody, a birthing person, up to 42 days postpartum that's related to pregnancy.
It's the metric that's used by the World Health Organization. Pregnancy-related mortality is a metric used by the CDC, and it's something that they monitor quite closely. These are deaths during pregnancy and up to one year postpartum that are related to pregnancy.
And then the broadest group is called pregnancy-associated mortality, and that's a death during pregnancy or up to one year postpartum from any cause. Next slide, please. So whether you're looking at maternal mortality or pregnancy-related mortality, you can see that we've had an upward climb and that our rates are too high, and they're not good.
Next slide, please. Now this is data from the CDC showing you the pregnancy mortality ratio for each state and also Washington, DC. And what's striking about this slide is how much variation there is and that the risk of a pregnancy-related mortality can be three times higher in one state than another. Next slide, please. And as you heard there, as reflected in the previous slide, there are striking geographic disparities.
Now this is data from about 2011 through 2016 from the Pregnancy Mortality Surveillance System from the CDC that really tried to look at rural versus urban pregnancy-related mortality and really showed us these significant disparities. As you can see on the right-hand side of the slide here, that in rural areas, the rates are much higher than in urban areas and, in particular, large metro areas. Now this is very consistent with the data that we know about rural healthcare and access to maternity care. In fact, there's limited access to healthcare services during pregnancy and childbirth. We know that individuals have to travel longer distances to receive maternity care, and more than half of rural counties have no hospital that provides childbirth. Next slide, please.
And another really important part of this story are the significant racial and ethnic disparities that exist. Here are pictures of three women that died from a pregnancy-related cause. In the upper right-hand corner is Dr. Shalon Irving, and you may have heard her story when NPR and ProPublica did that series on maternal deaths in the 2017, 2018 timeframe. She was a CDC epidemiologist.
She delivered her first child by cesarean, went home, died three weeks later from complications of hypertension. Now she was seen four or five times in those three weeks, complaining and having high blood pressure at all of those visits and still died. In the lower right-hand corner is Erica Garner, whose father was killed by the New York City Police. She became a big advocate against police brutality, and she died three months following childbirth from a heart attack. And then in the right lower corner is Rosa Diaz, who was featured in another NPR, excuse me, ProPublica story around Texas Medicaid and the uninsured and maternal health.
She died from a ruptured ectopic. She did not have health insurance. Next slide, please.
So you heard earlier this afternoon about the significant racial and ethnic disparities and the size of those disparities, and here's data from the CDC documenting those disparities. You can see that black birthing people are about three times, a little more than three times more likely to die from a pregnancy-related death as compared to whites. And you also see here that American Indian, Native American folks have a much higher rate, more than twice as likely to die from a pregnancy-related cause. Next slide, please. An important part of this story is the fact that these disparities have existed for decades. In fact, they've existed for black, the black-white disparity has been in existence since we started measuring maternal mortality.
And here's a slide from something published by the Commonwealth Fund showing Eugene Declercq, showing the gap over time. And you can see that initially in 1916, when our maternal mortality rates were much higher, the gap was about two times as high. But over time as our maternal mortality rate has dropped, particularly in the 1900s with the introduction of antibiotics, et cetera, you can see that this gap has persisted and actually climbed to rates three, four, and five times as high for black versus white women and birthing people. Next slide, please. It's very important to recognize that these disparities are not explained by socioeconomic status. Here's data again from the CDC showing us that a black woman with a college education is more than five times as likely to die from a pregnancy-related cause as compared to a white woman.
Next slide, please. You can also see that a black woman with a college education is 1 1/2 times, more than 1/2 times, as likely to die from a pregnancy-related cause as compared to a white woman with less than a high school education, in blue on the left-hand side of your screen. Next slide, please. So what's killing women? Now, this is data from 14 maternal mortality review committees across the United States, and they summarized the underlying causes of death by race. And here you can see for black women in these 14 states, cardiomyopathy, cardiovascular conditions, and preeclampsia, and eclampsia were the major killers, versus for white women, it was mental health conditions that included suicide and opioid use, cardiovascular conditions, and hemorrhage. Next slide, please.
And here's CDC data showing us, overall, for 2007 through 2016 what were the leading clinical causes of pregnancy-related mortality. And again you can see that cardiovascular conditions really are the main culprit, infection, severe bleeding, cardiomyopathies, blood clots, high blood pressure. Next slide, please. But an important part of this story that we really need to also recognize is that there's rising rates of maternal self-harm deaths. Over and over again, we're hearing maternal mortality review committees from across the states indicating that suicide is a leading cause of death among new moms. And we also know that the opioid crisis has dramatically impacted maternal health.
We know the rates of overdose deaths among women have increased. We know opioid use disorder has gone up more than four times among pregnant women. And we know that this rising rates of opiod use is dramatically impacting infants with rising rates of neonatal abstinence syndrome. Next slide, please. Another really important point of this story that I wanna make sure people recognize is the timing of death.
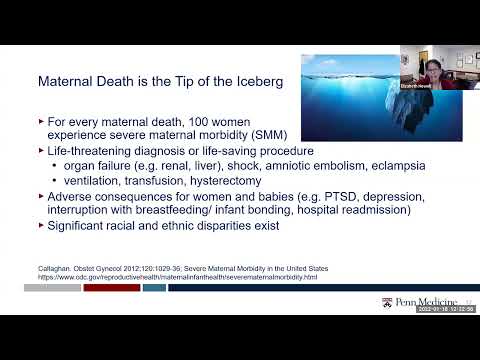
We've learned so much over the past number of years. We used to think it was mostly around that third trimester of pregnancy and during delivery. And maternal mortality review boards as well as data from Europe and everything, we've really started to recognize this is a continuum and the truth is is that greater than 50% of these deaths are occurring postpartum from day one through the first year postpartum. Next slide, please. Now a maternal death is just the tip of the iceberg. For every death, over 100 women experience a life-threatening diagnosis or undergo a life-saving procedure.
These are things like end organ failure, kidney, liver failure, shock, eclampsia or seizing, having to undergo a hysterectomy because you bled so much following your delivery, and you have to lose your uterus. So not only are these significant complications at the time of delivery. They also can occur postpartum. And there are significant consequences for women and birthing people and babies that go beyond just these complications, such as post-traumatic stress disorder, which there's growing data indicating that, for example, women who have undergone a hysterectomy, unexpected hysterectomy during delivery, have PTSD, depression. There's interruption with breastfeeding and infant bonding, and many, many have hospital readmissions or ED visits.
And similar to what we've shown for maternal mortality, there are significant racial and ethnic disparities in severe maternal morbidity rates. Next slide, please. And here is data, national data, showing us for some of the underlying diagnoses associated with severe maternal morbidity, you can see there are significant racial and ethnic disparities.
Blacks are in darker gray, and American Indian or Alaska Native are in the darker blue color. And you can see that across many of these underlying diagnoses, there are racial and ethnic disparities. Next slide, please. Another important part of the story is not only the significant morbidity and associated consequences for people having children and birthing people in our society, but there are significant costs, not only just for that individual delivery that's associated with severe maternal morbidity, but there's so many additional costs postpartum, lost work, all sorts of things. And this is a report that was done by the Commonwealth Fund that tried to quantify the cost. And you can see that looking at both maternal and child outcomes for up to five years, they cited a number that was greater than $30 billion.
And that again is only for the top-nine underlying causes of severe maternal morbidity. Next slide, please. So how did we get here? Next slide, please. So I'm a health-services researcher, and I think about things, factors of the patient, community, clinical, clinician, and system level.
And I wanna start this discussion by recognizing that as there's growing recognition in this country with COVID, with George Floyd, and everything that's happened, that these disparities are rooted in structural racism, the policies and procedures that have been around for centuries in this country and their impact on the way that we live our lives and our health. It's not about an individual's race but rather how society responds to that individual. We can think about patient factors, such as poverty, insurance, marital status, language, knowledge, beliefs, health behaviors. We can think about psychosocial issues, such as stress, the weathering hypothesis, the idea that the stress from racism and how it impacts birthing outcomes, social support, community, and neighborhood factors such as social network, built environment, crime, clinician factors, such as knowledge, experience, cultural humility, implicit bias, as well as system factors, access to high-quality care, transportation. These combine and set a person up for their health status when they become pregnant.
Individuals can have comorbidities such as high blood pressure, diabetes, and obesity that put them at a greater risk for severe maternal morbidity and mortality. They interact with the healthcare system preconception, antenatally, delivery care, and postpartum. Next slide, please.
And really important here is to say that maternal mortality review boards have shown us over and over again that greater than 60% of these deaths and a sizeable portion of these severe maternal morbidities are preventable. And this slide also echoes something that you heard earlier about life course and realizing that it's across this care continuum that we can intervene to address these outcomes. Next slide, please.
So here are some levers to reduce disparities and improve outcomes from a quality-of-care perspective. Next slide, please. First, we need to think about the preconception period, optimizing health, managing chronic illnesses such as diabetes and hypertension, and promoting culturally appropriate contraception. Next slide, please. There are new models of antenatal care, such as group care, medical homes, enhanced models for high-risk women.
Next slide, please. Quality improvement, standardization, and the use of bundles on labor and delivery units so that we standardize care and make sure that every woman or birthing person who comes in with high blood pressure is getting the most recent evidence-based practices. Protocols, disparities dashboards, where we stratify quality metrics by race and ethnicity, and ensure that all of our patients are receiving high-quality care. Next slide, please. And then in the postpartum period, patient navigators and case managers thinking about ways to connect our patients with care.
But just like you heard about Dr. Shalon, or maybe you've heard Serena Williams' story and so many others talking about not being heard, we have to think about additional elements. Next slide, please. Eliminate bias.
Next slide, enhance communication, next slide, and engage community. And I wanna say to this audience that's thinking about technology, there's a role for you to think about the use of technology in all of these areas across the care continuum as well as when we think about bias, communication, and community. Next slide, please. So how can technology help us? Next slide, please. I wanted to start this conversation around technology, thinking about a couple of themes, first, the care continuum, preconception, antenatal, delivery, and postpartum, that we need to think across this care continuum as opportunities for intervention and improving outcomes. We need to be thinking about the social determinants and how they impact maternal health outcomes from the built environment to nutrition.
We need to think about quality of care, which is the angle that I often think about, and I showed you sort of the thinking and the way I think about it for levers to reduce disparities and also improve outcomes. There is a lot of opportunity for technology in this space. And then the other major area that I wanted to make sure we think about is communication.
There are so many communication failures, whether it's between the patient and the provider, the nurse, the physician, and the midwife, individuals not feeling listened to. Over and over again we've heard these themes, and so anything that we can do to enhance communication, these are all critical areas when we think about maternal health. Next slide, please. When individuals have looked at these maternal mortality review boards and looked at what are the themes, the themes that seem to come up over and over again in these deaths, inadequate assessment of risk, failure of communication, failure to screen, ineffective treatment, delay in diagnosis, treatment, follow-up, lack of coordinated care. So when we think about those areas, we can start to think about, okay, if we had big buckets, what are the things we really need to be thinking about? We need to think about communication, as I mentioned.
We need to think about education, not just for patients, educating them about risk factors, all those kinds of things, but also around the provider side, education around bias, education around clinical care, education around disparities. We need to think about how we engage patients, get them connected more in their care. That's a really important area, screening. We need to come up with better predictors, predictive modeling to help us identify those who are most at risk. Next slide, please.
Care coordination, we need to think about this incredibly fragmented care system that we have that so many people are seen in one place, end up delivering in another, and their medical record doesn't follow them, or people don't know what's happened. They've seen so many care, different providers. The importance of standardization of care and making sure that evidence-based practices are used and that we're delivering the highest quality of care to all patients throughout the care continuum. And then we need to think about implicit and explicit bias and what are the things that technology can do to help us reduce bias. Next slide, please.
But we also have to think about the challenges to the use of technology. We know that lower socioeconomic status and individuals of color are less likely to engage in internet health-seeking behaviors. For example, in a study of low-income women that had about 14 focus groups from the Midwest and East Coast, while they found a very high access to smartphones and the use of internet, they found low use of internet or other digital tools for health-management practices.
Studies in the general population as well as in pregnancy and postpartum women do reveal high access to mobile phones, but we also know many phone numbers change within a year. The use of digital health-management practices is low, and another study of about 250 women, again, of pregnant and postpartum women in the Baltimore area, found high mobile and texting use but found less internet uses, especially around disparities. So while we think everyone is doing this, and everyone has it, they actually found that English-language proficiency, education, health literacy were all associated with use. So if we don't focus on equity, usability, and user preferences in this space, we could inadvertently widen racial and ethnic disparities.
So I want to really stress that to this audience. And in a paper that I read by Steinberg et al., and I don't know who originated this. You guys in this technology audience will tell me about digital inclusion, but it really struck me, this notion that when you are developing technology in this space, you have to be thinking about access, equity, and justice to make sure that you're reaching all those people who are often left out who have the highest burden of disease and, in this case, the highest burden of morbidity and mortality. Next slide, please.
So there are a number of tools that we can use to address maternal health across the care continuum. And you guys are familiar, and you're gonna hear more today about many of these. There're growing studies that indicate health IT tools are incredibly important.
Electronic health record, clinical decision support are important for populations that are underserved. Improve implementation of clinical guidelines, promote patient safety, provide alerts to healthcare teams of patients who would benefit from targeted preventative or therapeutic interventions. They facilitate standardization of care and can reduce disparities.
You all know that telehealth has been so critical during this COVID crisis. We thought of its use a lot for rural, for maternity deserts, for folks in rural communities. But we found even in urban settings how important it's been. Here at Penn at the Hospital University of Pennsylvania, we found for our pregnant patients that actually we reduced no-shows. So for a lot of our lower-income patients, they were able to attend visits through telehealth that they would not have been able to because of transportation barriers, work, et cetera. We know there are wearable devices, and a lot of people are in this space.
I think many of you have probably heard about power moms that collects pregnant women's data, like surveys, and uses wearable technology. There are a lot of folks in that space. Mobile applications, hundreds and hundreds of these apps that allow black and brown patients to create reviews of their OB-GYNs, birthing hospitals, to tech startups such as Mahmee, that connect new moms with healthcare and support, offering tools like surveys to assess their postpartum emotional and physical health. And I think with Serena Williams' endorsement, that has gotten a lot of notoriety, but there's so many more. Wanna emphasize the importance of data analytics, predictive modeling. I mean, use of machine learning to identify patients who are most at risk for early intervention is so key.
There are so many areas in which we need to work on this. And then I also wanna talk about and remind everyone about how important it is to have tools in care coordination space. We need to use technology to reduce fragmentation of care, increase engagement, and keep women connected to the healthcare system. Next slide, please.
So I thought I would just share a few things that we're doing at Penn, just to give an example of some things that we're doing at the bed with our patients to improve outcomes in maternal health and in the Philadelphia area. Here's a program called Heart Safe Motherhood that was started a few years ago by Doctors Hirshberg and Srinivas. And it's a home postpartum blood pressure monitoring program that leverages technology and essentially allows birthing people to go home with a blood pressure cuff, and they text their blood pressure results. And they have a texting process, and there's an algorithm for referral. They did an RCT and found that there were increased blood pressure measurements in the first 10 days postpartum to those who were a part of the intervention group, reduced ED visits and readmissions, that there was a decrease in disparities that many more black patients than before were actually getting their blood pressure checked within those first 10 days, and increased postpartum visits. It's now at all five Penn delivery hospitals, and it's actually being disseminated and implemented in all Philadelphia downtown delivery hospitals through our Philadelphia Department of Health in a grant they received.
Next slide, please. Another program called THEA, Text Message-Based Antenatal Educational and Blood Pressure Monitoring. So now we're giving a blood pressure monitor to all of our OB patients at our Hospital of the University of Pennsylvania in our generalist division. They get weekly educational text messages before even their first prenatal visit. Then they get the blood pressure cuff. They get access to a number of articles and videos hosted on an educational website.
And then they have weekly blood pressure monitoring beginning in the second trimester with an algorithmic triage of abnormal values. And what Dr. Graseck, who developed this program, has found so far is that at least 80% of patients are submitting one blood pressure, that we have a very high-risk population with 41% of patients being diagnosed with gestational hypertension or preeclampsia, remember noting that the general public idea is around five to 8%. Around 8% is what you think.
That it really facilitated reduced prenatal visits during peaks of COVID by incorporating telemedicine visits, and that 60%, this was really critical for us, 60% of the elevated blood pressures in pregnancy were first diagnosed using the home cuff, not in the office. Next slide, please. We have another program called Healing at Home by Doctors Kirstin Leitner and Lori Christ bridging the gap in the fourth-trimester care. And really this is a combination of anticipatory guidance, two-way texting, and support for lactation and postpartum depression screening. A texting or chat bot uses natural language processing and augmented intelligence to coordinate care, provide resources, and address issues, answers questions, and connects women and birthing people to their providers when necessary. This program has been essential to us during COVID, allowing for 24-hour hospital discharge following delivery and a mechanism for us to provide needed support and needed care for folks after they've delivered.
We found really high engagement, a number of patients asking questions about breastfeeding and completing the surveys. Next slide, please. Remote fetal monitoring, one of our investigators here, Dr. Schwartz, has a collaboration with Nuvo, which is a self-administered sensor belt, to really try to do at-home, remote fetal monitoring. And just to remind this audience, there are about 26,000 stillbirths every year in the United States.
And we know there are a lot of barriers for pregnant women and birthing people to actually come into the office, those high-risk ones who really need this fetal monitoring, to try to prevent the occurrence of these stillbirths. We know that childcare, time off work, and transportation get in the way. And we also know that black women are twice as likely to have a higher risk of stillbirth. So this is an opportunity to try to think differently and to try to reduce disparities.
And, in fact, Dr. Schwartz recently was funded by NIH with an R01 to work further on trying to target disparities in this space. Next slide, please. I'd like to talk a little bit about a program here in Philadelphia as one more example of a program that's leveraging technology, really focused on low-income women and birthing people to try to optimize health outcomes in the maternal-care setting. It includes a multidisciplinary care team, a maternity navigator, in-home and virtual visits to meet patients where they are.
They leverage community and work with community partners, and they leverage technology through something they call the Cayaba Brain, which includes EMR, claims data, questionnaires. They use this data source to risk-stratify and personalize care and to support the multidisciplinary care team. And according to their website, they have found that really high engagement, high satisfaction, 35% reduction in emergency room visits.
And they have found that the people that are involved in their program are three times more likely to attend their scheduled OB appointments. Next slide, please. And then I wanted to end by just reminding everyone how important it is to think about all technology and the use of data-driven modeling. Whether it's around building models of pregnancy biology, or whether it's around predictive modeling to try to help us better understand who's most at risk, there's such an opportunity. We have data streams for so many things, genetics, environment, nutrition, medical history, stress. We know there's so many sources of this, and we need to put this together to help us optimize health for patients.
And one of the things that I'm working on right now is a predictive modeling with my research group around trying to identify who's most at risk postpartum for an ED visit or postpartum readmission as a marker of severe maternal morbidity and mortality and then how can we intervene to reduce its occurrence or their occurrence. Next slide, please. I'll end with this quote by Dr. Lisa Cooper: "Most health disparities are avoidable.
They result from decisions we make as a society regarding how we allocate our resources and how much injustice we are willing to accept as a fact of life." Next slide and next slide. And remembering digital inclusion, that we need to think about equity and justice when we implement technology solutions. We need to think about how they impact all patients in our population so we can reach those who have the highest burden. I think we need to think about these themes of communication, engagement, education, screening, care coordination, and standardization, and bias. Again, social determinants of health, quality of care, and this care continuum are the main messages I wanna leave you with as you think about technology in this space.
Next slide, and I'll end there. Thank you very much. Thank you, Dr. Howell.
That was a really great talk and really eyeopening. Very much appreciate it. Do you have time to take one or two audience questions? Yes, I do.
Okay, so if there are audience questions, please use the raise-hand icon at the bottom or send a message in the chat. And while we're waiting for one or two audience questions to come through, I'll just start us off. I really love the theme of how you talked about, we have to have best practices with the technology that we develop for achieving access, equity, and justice. What are best practices that we can do to make sure technologies develop that way? How should we start thinking about it? Well, I think about it more in the, I think you have to do a lot of reading. I didn't mention this, but I have not been a person who's worked a lot in technology. I have really worked much more sort of in the quality-of-care space.
And I was so struck when I did a lot of literature-searching around how many people are really being thoughtful and thinking they're getting data, talking to women and birthing people to try to understand what's most important to them, how might they be best engaged in the process, and what are the gaps that we know about? And I think starting at the end user, understanding their preferences, understanding how they use things, what are the barriers, how might we help people, we don't need a fancy thing a lot of times. We just need something that works for people and especially for those who often aren't represented in these audiences. Thank you so much. We have a couple of audience questions coming in.
What fraction of maternal deaths do you think can be averted with pregnancy postpartum treatments versus lifelong treatments? The are lifestyle (indistinct) for pregnancy. That's a hard, hard, and excellent question. So, you know, we know that a huge, significant chunk, as I mentioned, over 60% of these deaths, are thought to be preventable.
And there's a lot of space for quality of care because remember I talked to you about the delays, delays in treatment, delays in diagnosis, all of those delays, as well as communication failures. So I honestly believe we could do a lot in the care setting antepartum, during delivery, and postpartum in that space to really reduce maternal deaths. But there is no question that this is a life-course issue. It's around optimizing health preconception. And as you saw in the slide earlier from the time in the womb all the way through, I'm a real believer that it's the life course we have to really apply our thinking to if we're ever gonna change this metric in this country. Thank you so much, and we'll have one final question 'cause we're running over time.
But you talked a lot about technology that was being implemented at Philadelphia, where you are located. Are there support for replication of these models in other states, thoughts about expanding these models and making them larger since they are now shown to be working? Well, so thank you so much for asking. We have a Center for Healthcare Innovation here at Penn in the School of Medicine, which we partnered with for these various programs. And they have been a great partner for us, and we continue. So the Heart Safe Motherhood program right now is being implemented in, I don't have the exact number, but a few programs across the country.
And there have been a number of people that have been working together with Doctors Hirshberg and Srinivas 'cause they're trying to disseminate it and get it out there. Our other programs are a little bit earlier in their trajectory, but our hope is that as we find that these things are effective, and that's one of the things we're very committed to, is finding out, measuring and finding out and evaluation, and making sure that these things are productive and helpful for patients. Once we get to that point, we will continue to try to work towards broader dissemination. Thank you so much, Dr. Howell. That was a really great talk. We really appreciate you being here and part of our workshop, and we really hope we can continue the discussion with you.
Thank you.
2022-02-17 23:48


