TRACO 2017: Genomics and Lymphoma
Our, first speaker today is June way, he's. In. The, uncle, genomic section, of the genetics, branch, he. Got his bachelor's degree at the University, of Houston and, subsequently. A PhD. At Baylor, College of Medicine and. He. Did postdoctoral training, in Paul Meltzer's, lab and. Currently. He, assists, Javed Khan and, he does the ongoing, research in, the, onco genomics section, so, as titled today the application, of genomics, to identify, diagnostic. Biomarkers. Drivers. And therapeutic, targets, for pediatric, cancers June, yeah. Thank. You teri for the. Invitation, to gave, this lecture and. Here. Is an outline of what, I won't going to do today, and. The first I'm going to introduce, you what, is a success. And the challenges, of treating, pediatric cancers. And. The, second. Topic. I want to introduce. To, you is the genomics, and the. Third, one is the next-generation, sequencing. Which is the powerful genomic, tools recently. Developed, and the, way are extensively. Using, these tools to. To. Study. Cancers, and. Next. Part is are. Going to give you some K, examples. To show what's, the application, of this next-generation, sequencing. We, can use the undiagnosed as. A diagnosed. Diagnostic. To and we. Can also attend, identify. Molecular, targets for treating those cancers, and the. Last portion I'm, going to get. Into the precision. Medicine which is. The. Very. Important. Area of the medicine, to, use this genomic. Tools to. Make, the precision, medicine a, reality. So. This, slide shows that the. Pediatric. Cancer, it, is actually it's a very successful story. You, can see in the 60s, which is depicted, by the blue. Bars the. Survival, rate for, these. Three. Pediatric. Cancer is a very low but. In the nine days you see it's a there's, a dramatic. Improvement, of. The survival. Rate for. The. Cancer. Patient, with those cancers. However. In. The, past 16, years you, can see this is a mortality rate. Decreasing. This is a limb. For limb. For lymphoma and leukemia and, this, is other pediatric. Cancer, and you, can see, they. Are decreasing but. At. The body year 2000. This. Decreasing. Start, to level of data, means, expect. A lot of a very. Aggressive. Therapy, and, actually. Those therapy. Is very not. Only aggressive but they are very toxic and. But. The mortality rate, is still. Keep a certain level, so. That's the problem. Facing, to the nard. A more than modern. Oncology. In Pediatrics, and. If. We look into the detail of those. Survival. Data. We, find that, the. Most patient. Cannot, be cured. With. The pediatric. Pichette. Pediatric, cancers I'm at metastatic. Recurrent. On the refractory, disease and. The. If. You look at the neuroblastoma is still, like 30 40s, and. Then you. In suppose a coma the survival, rate down. To 20, 30s and this. Is a rhabdomyosarcoma.
Magma. Tastic. Rhabdomyosarcoma. And. Osteosarcoma. You, can see all this high stage, means. The metastatic. And, the recurrent. Tumor, the cure rate is still pretty, low. This. Is the challenge of this. It's. Pediatric. Cancers. Okay. So we, have this phenotype, and how. Do we, study. Those with. The modern, technology and. These. Slides show you that the. Relationship, between a, genotype. And phenotype. So. You, can see this is this is a, caterpillar. And this is a dog, a butterfly. They. Look so different right. But. They, share the exactly, same genome, okay. So. This. Is the same genome, but they have very different the, expression, pattern and different, the proteome, and the, different tissues and they have different, physiology. And. Odd. Is the, summary. Of this is the phenotype right, so. This, is also apply, for, the human okay although human. We all have, the same genome, but. In our body would, have so, many different kind of tissues, it's all coming, from this same genome, so. From, the same genomes, we can have skin in, a, different, the glands and, the airway, epithelial times. So, and so forth, muscle. Cells neurons. You. Name it this is a, very. Very, different cells, and the tissues but. Yet, they all share, the same genome. They are encoded. About the same and DNA. Okay. So. These account complexity. And the diversity, is all. Resulting. From, this genome. Okay, it's, encoded. In the genome. And. This. Slide actually it's depict, the. Central. Dogma in, biology and, this, is the. Information, flow is from the DNA, and that, one dearme transcribed, into the RNA, a messenger. RNA and then is then. Translated, into the protein, and the, protein, where. Many is, the what we saw is the phenotype. However. This, not at the same port there's a lot of feedback loop back. To for, example protein. Can control, the. Translation. On stability of, the, messenger. RNA and also. Protein can control the genome, to, determine, when the gene is on, when. It's off and how much is the arm how, much the. Expression. Level is so, this is all. The. Feedback loop, under recently, we also discovered. That there's a group. Of, RNA. Called micro, RNA, and they. Themselves. Is, not, coding, that you do not coding, for protein. Or other things, but, they have very, important. Regulatory, roles, for. The transcription, as well as the translation. So. This is a very, complicated. System. But. This. Is a very it's. A simplified, version of the complicated, system but. You can have, some sense, the, information.
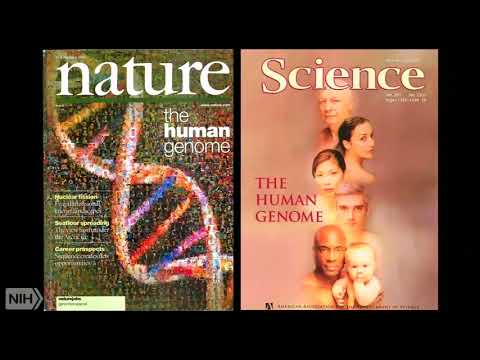
Flows, Is, from the DNA, to, the mRNA, eventually, to the protein, and. This. Is the rough. Line to. Separate. The, study. You know this side we. Study the nucleated, nucleotide. The acid, of DNA, or RNA. And. Then we call the genomics, and this, part we started, protein. Which. Is called protein. Proteomics. An. Interim. Of number, we know that, human. Genomes, code. About, 30, billion. Has. 30 billion base pairs right and the. These, 30 billion base pairs only code for about the 25, to 30 thousand, genes. And this, is it actually, it's a kind of surprising. When the first. Of human genome project, finished, and that they, originally. Expected, a much more dings but. It turned out is only 35. To. 25. To 30,000, genes however. There's, a lot of for, each genes they can have different. Ising variants, right, so, the estimation, for this, all this price variance, is, about a hundred fifty thousand. Three. Billion. Sorry. Oh did, I see 30 sorry, three, billion base pairs yeah and. The. Small micro. RNA, there's about a thousand. Or so, micro. RNA and also. There's about it over. Ten thousand, the, encoding, RNA, those are other regulatory, elements. To. For. The regulation of, the genome. And. In. The protein. Side is. Estimated. About a half million. Proteins. But. On the, on the top of the complexity. These, are 50. Or. 500, thousand. Proteins, they, can have a different form for example they can be phosphorylated. They. Can be methylated. So, on so forth there's a modification groups, towards. That and the, word change their functions, and their activities. So. That's the whole. Very. Like a 30,000. Foot. Overview. Of this, biological. System so it's a very complicated, system. And the, information, flow, is. Is. Programmed. By. This genome. And it's. Very precise, and the. In terms of the timing amount. And the place spatial, expression, it's. All, programmed. In the human, genome and. Recently. The data shows, that although, only, one, or two percent is the coding, sequence. Coding, these twenty, to. Thirty thousand, genes right but. Eighty, percent, of the human genome actually, is transcribed. So. Before. People always think that the most, human. Genome is full of junk DNA but. Now we realize, these these are not junky, and eighty percent of the human genome actually, functional, yes. Correct. That's who from the encode project 80%. Well. You. Can cut the crap but it is a incredible. Information. From, the encoder project you know and we understand, a lot of things recently. About. The epigenome. Epigenetics. Modification. All these kind of things all from the uncle project. And the it. Reviews. There's much more information than, just a transcript. Transcribing. Rnase. Yeah. The come the, complexity. Of this system is so huge, you, know we do not understand. All of them that's, reason before we think this is our job DNA, actually you, know not necessarily yeah. So. This is the first. Milestone. Of the human project right, by. 2001. I think after 10 years the launch of the human project and then, we have a first, draft of the human genome. So. This is a like, both Journal, has this. Debuted. For this completion. Of the human genome in 2001. Under. The. Genomic. Research, in cancer actually, take. A. Huge, advantage, of human, genome of the information. Regard because the human genome gave us a complete, map, of, genetic. Code that we can study with and make, a lot of. Research. Project, much, easier. Than. Before than, before the human. Human. Project, I just, give you a simple example you, know when I was a graduate, student. We. Discovered, a gene called, a category 11 at that time we. Won it's only 6, 1.5. KB gene ok it's very short we. Want to sequence it it took me almost, two years the. Render, you, know the Sanger, sequencing. Gels, jail. Of the jail to sequence that. 1.5. KV but. Nowadays, you. Can sequence the human genome overnight. Three, billion base pair so that's the power. Of the technology okay. And. The. Way we use human, genome. That. Is the genome. Map is we. Use. This technology, to. Also. The information, to identify, the biomarker. And hopefully. Those biomarker. Is the. Driver of the disease and then. We can device, using. The. Using. The you. Know either drugs, or, synthetic. Compounds. To, interfere, with this disease. That's. The therapeutic. Target, and. Also. All this, hopefully. They will be low or no. Expression, in the normal tissue so do you do not interfere, with the. Normal, function, of our body. Okay. The challenge, of this kind of a complicated, disease. Like, cancer is how. To measure, and detect genes and their problem, in a massively, parallel way, because, if we have you, know so many you. Know tens of thousands, of genes and. This. Is really, the genomics.
Comes. In and the genomics, is using. The high-throughput. Technologies to. Deal with this problem, and this. Is in hand with. The. Technology, in the computational. Technology. So. We need have enough, computational power, to do that before. The computer. Have. Enough, computational. Power. This. Kind of study almost is impossible. Right you you. Can generate data but you cannot process, yet but now we, have the power to. Process. This kind of data. And. These. Slides just show you the, first generation. Genomic tools this, is the color microarray, and the. It use, are different, the kind of method, to printing, the probes DNA, probes on. Glass. Slides or some solid, surface, so, that these. Probes. Can be. Physically. Fixed, on particular. Spot okay. And, here, I show you some technology. Common technology, for example you can use the mechanical this, is like all, these little pens they are like a quill pen the. Dip into the solution, and the printer on the slides and. This one's more advanced. Is it you see electronic, a piezo this. Is like the inkjet right, we. All use the inkjet printer, this is the same kind of technology, you can inject, printing, those probes on the glass slides and. Later. There's, a more, advanced. Technology. Used look at the. Little. Graphic mask. This. Is the same kind of technology, to make the computer, chip. So. Affymetrix. Using, this kind of technology, to, make their. Microarray. But. This. Technology. At the very beginning, they have to generate, a physical mask, in, in other word it's the. Physical. Mask. To, let either. LED lights loop through, or, blocking. The lights this is a physical mask if you want to generate a 20, something. 20. Murali goes you need to generate at least the twenty-something, masks to, do this and, this is a very costly and the. Later they, use this digital. Mirror, micromirror. Technology widget. It's exactly. The same technology, as we are using on in the digital projector. They. Can project the light to. The place they want they, intended. To to. Finish, this. Graphic. Chemical. Process. So. This is a microarray, and. If. We have a piece of microarray. With. The odd is the different the probe we know what. The probe sequence, is and, we. Can label. The, samples, either, from our health tissues, or cancerous. Tissues, with different the fluorophore and, they will put into the solution, hybridized, into, this array and this, hybridization, happened. To, specifically. The. Probe where specifically, hybridized, to the target. And then, we can use like. Can. Franco confocal. Microscope. To. Scan, the slides to get an image and the intensity, of each spot, will. Indicate, the. Signal, the, original. Abundance. Of the molecule, in the original sample this is the, microarray to how the microwave, works so. It's a technology by, hybridization. But. Lately we, have a new, to genomic, - it's called the next generation, sequencing, and. In. This technology, what. We do is just basically, it's a shotgun sequencing, so. If you have a biological, sample, either DNA, or RNA and. This. These, technologies. First. The will do the sharing or, fragmentation. Of this, molecule, i turn. To a small, different, size and then, after, size selection you put the adapter the common, adapter, onto end, of this DNA. Or RNA fragment. And you, can sequence those. In. A massively parallel. Way, and then. You'll align, all those little sequences. To the reference, genome reference. Human, genome and, then. You can. Reconstitute. Original. Sequence from, the sample, okay, that's just the, principle. Behind this next-generation. Sequencing. And. Is a real, picture, of the. Image, coming from the next generation sequencing, this is a field all, these little dots is one.
One. Cluster of DNA, strand okay, and if. I we blow up this, little square you can see this is a very dense, clusters. Of different, DNA. Strands, so. Each spot, is. Equivalent, to one Sanger, sequencing, so. In. The same time this, is that reason it's called a massive, parallel, sequencing you. Can sequence. Hundreds. Of millions of those DNA. Under. The image, I just show you it's about this, size on a whole, flow cell okay. So, you, can imagine you, know, with these four lengths of flow, cells you can have you can acquire a huge, amount data, in. A very short period of time. Okay. This slide shows, what. Kind of information we can get from this, kind of technology okay. And the, first thing we can get the point mutation. If, we align our reads, we, compared, to the reference genome we said hey. This, supposed. To be a a but it's a C so. We, know there's a mutation happen, here and, also, we can find the, India. Which is a small, insertion, of the deletion and. All. The reads here, it will be in. This case will. Do. Not contain, the sequence from this side right and, if. There's a bigger. Region. Of deletion. If he's a, homozygous. Deletion. You won't see any Rita at all but. If it's a him. Azygos delusion, you will see some reads but not as many. Reasons, as the adjacent region. And, again. If it does again you can see this more reads than it should be right, and. Another. Thing is. The. This, kind of reads, contains. On the same model, contains, the sequencing, coming from the different part of the genome in this, case from the chromosome. One as well as chromosome, five which. Is unusual, that. Reason we can detect. The translocation, and the breakpoint. You. Know all those kind of things if, we want to detect, in the in the past it's, a pretty laborious, process. You, have to clone it out you have the sequence of one by one it's. Very laborious but. Now you can, do everything very quickly and another. Thing is you can also detect, the pathogens, in your sample, for example some tumor, is caused, by the pathogen. Like, the human, populace, virus. Will cause the cervical cervical, cancer and actually. From the cervical cancer, samples. You. Can detect, this kind of pathogen. Which is not a human sequence. This. Is on the DNA side and the. Same oil with the RNA, and. Using. This technology, we can acquire, digital, expression. From. The RNA samples, and we can also detect, Express, the mutation. Alternative. Splicing, event, and the. Fusion, events. And the. RNA, editing and, novel. Transcripts, and then, coding, RNA, okay. And. The advantage, of the next-generation, sequencing. Technology. Versus, the microarray. Is there's. No need to prepare clones, for the DNA fragments, right and there's. No needs of prior. Knowledge of, the probe design, because the further all the DNA. Microarray. If. You want to detect something you need to know what. Do you want to detect then, you have the design, specific, probe for that things for. Example if there is if there is a fusion. Gene, which. Is not a naturally, happen, if you do not know it's very hard to design. Some probe to catch the diffusion, part. And. The. Another advantage. Is sometimes. Even the microarray you can have. Some indication. Of. Gain. On the loss of. Genomic. Genomic, material, but. If he's a balanced. Translocation. For. Example just the two chromosomes, eyeing abnormally. To each other on the, microarray. You cannot detect that event because it's a balanced, but. In the in the next generation, sequence indefinitely, and it detects such event and. It's. Because it's a, sequencing. Based you, can generate, the base pair resolution data. So immediately, you can know where's. The fusion ad where's, the mutation, had you don't need to. Collect. The like, the past you have the map to the chromosome, try to do, the linkage study and, the. Ways. The technology, getting mature and the mature and the. The sequencing, actually is become cheaper, and cheaper and. The cheaper and the and the faster, per genome cost. And. The, date this next-generation. Sequencing. Is also, can. Allow. To. Acquire, all different, kind of information use, the same platform you, can in, in in. The past if you do microarray. You have the design different array you know for the copy number array, snip array and the expression, array or different kind of different array but. For this next-generation, sequencing. You just need the same just. One sequencer, and depends. What, kind of a library you make you can get a different, kind of information, for, example for. The DNA, said we. Can get a whole genome sequencing, and, you. We can use the whole exome, sequence in which you use the probe just to put on the coding region. And. The methylation, sequencing. Your only sequence, the. Places. CPG, Island, that is rich, with, the, events. Of the, methylation, and also. You can do the chip seek chip, seek which. Is food, on the transcription. Factor, binding, area to, say where's, this transcription.
Binding, Specifically, and, the. RNA, you can do the messenger, RNA sequencing. And coding. RNA. Sequencing, and that, this is all the information you can get DNA. Side as, I said is a copy number, gene rearrangement. And. The. Entire. Genome. Or. Some. Novel, trans. Methylome. Or epi genome, sequencing. And we. Can also easily, detect. The damaged, mutations. Under. Our knee side again. There's. Information. For the gene expression of, the sample, and the chimeric genes space. Varian. Novel. Transcripts, and. The damage mutations, and the others, we. Can to, identify the biomarkers. And then. Understand, the biology of the cancers, and hopefully. We can identify the. Therapeutic. Targets. So. Here I give you an example, using. Genomic, tools to. Deal. With the clinical, cases and that. There is a. Four. And a half year, old girl. Sought, for second opinion, from pob and this. Is the formula and germany. And. Their. Concern, is the questionable, diagnosis. Because. The. Discourse. Cancer. Is not responsible. As. You should be as the diagnosis. And. This. Disco, has a six week of history, of weight loss and reduce the appetite, and. A fever and the abdominal, pain and the. On examination. There is a big, abdominal. Mass, showing. This mRNA. MRI. Scanning. This is the mass and also in the. Vena, cava there's, also a, mass. So. The initial diagnosis, is a Wilms, tumor, okay. However. When, we run a microarray, experiment, this is like a almost. 15 years ago when. We ran the. Microarray. Gene. Expression, profile this, is a. PCA. Plot. To. Show different. The diagnosis, group you, can see. This. Is a rhabdomyosarcoma. Expression. This is the, Wellness, tumor, and this, is a you, in sarcoma. This is neuroblastoma. And this is the, sample. We're talking about and. Instead. Of its grouping. With this Wilms, tumor actually groups. With the neuroblastoma, so. That's the reason we think this is another Wilms tumor at all, instead. We. Will revise. The diagnosis, into the new branch stoma and the, since then the, patient, was switched to a high risk in Europe a stoma treatment.
Including. The stem cell transplant, and the. Disco actually, doing pretty well after. A year at that time. So. That shows you how. Important. This you. Know what's the, application. Of the, genomic, tools can. Can, help in the clinical. Application. And. The. Since. Then we, we do not use the micro region much anymore, we, use the next-generation sequencing. In these slides you can see that. The. Next-generation sequencing, if we do whole genome we, can easily detect, this kind of a translocation, this. Is a from the translocation, happened. From chromosome, 2 to. Chromosomes, 13. Pax, 3, Fox. O1 translocation. It is, a hallmark for, the rhabdomyosarcoma. So. If you saw this translocation. You. Can very. Confidently, diagnosis. This is rhabdomyosarcoma, a. Same. Thing with this case it's a Ewing sarcoma has, a trend a. Hallmark. As. Location, between the comes, on 11 the 22, UW, is flying. And. This. Is, very. Easy also, using, the army seek, if. We look, at the RNA, we can easily to, detect those abnormal. Fusion, as. As shown. Here. In the indies, publication. So. About. Five. Or six years ago at that time the. Field. Of pediatric. Cancer, and there's. A lot of sequencing. Project. The going and the. We. The. The first result come out the from all those sequencing, big sequencing, project, is those. Pediatric, cancer, actually has a very low, mutation. Burden. Compared, to the adult cancer. These. Are the adult cancer, from, the melanoma, stomach, cancer so on and so forth you can, see it has a lot, of mutation. Per. Megabase, but when you go to come, down to the pediatric, cancer. Most, of them has a very few. Mutation. So. The question, at that time is, is there's any enrichment for, the action of mutation, mutation at, the relapse, of those, samples, and. His. Mutation, low the similar, similarly. Low at the read relapse. And the if there's any clinical, utility of, this. Kind of study. At. The. Especially. When the, patient. At the relapsed. Age and. What is the feasibility, and the performing. Genomic. Guided. The precision, therapy trials. In the pediatric so, that's the questions, we want to address. We. Designed. This study. We. Call it clinic. And that, the, chronometer is using, the state of state. Of art mod did, multi-dimensional. Integrated. Approach and to. Study, the pediatric, cancer. This. Is study design. It's. A pilot study and we. Try, to determine the utility, and the feasibility of performing. Comprehensive. Genome. Analyses. To. Identify, clinically, actionable, mutation. In the pediatric and, the young adult patient. And. In. This study we. Have 59, patients. Enrolling. Into. This ohmic, protocol, at the, the, pob branch, at the CCR, and, the. Time spans, from. 2010. To 2014. So. The, average age. Of. The patient they recruit is about, the from. Seven seven. Month very impatient. To twenty five years old and. It. Covers. About twenty diagnosed. Diagnostic. Categories. And. We. Perform, the comprehensive. Mod multi-omics. Exome. Germline, as, well, as a tumor, and the, tumor RNA. Sequencing, and. We. And. The in addition we also performed. The snip. Array, analysis. On those tumors, to get a copy number changing. Information. So. The first is what is the definition, of the actionable, okay, the. Actionable, definition. For the germline, mutation. Is the loss of function, mutation, or known hotspot, activating. Mutation. Of a cancer consensus. Jeans or, pathogenic. Or likely pathogenic, mutations. Defined. By the American, College of medical genetics. Okay. At that time there's a 56. Genes in. This category. And. The. Internal. The somatic, mutation, our definition. Is, genomic. Alterations. That changed the patient's, diagnosis. Or. Maybe. Targeted. About fda-approved, drugs, or in context, of the existing, clinical, trials, according, to the NCI. Adult match trial criteria. So there's a whole. Criteria, to, define, what. Kind of mutation, is actionable, or not if there's any trial, or drugs. Is. Indicated. By those mutations. And. Here. Is the overview. Of the data, generated. From this study and. Again. It's. Multi-omics. And, is integrated. The. Reason we said is integrated. Is shown as following, so. This part, of data you can see this, is generated, from the RNA, seek. And. From. Here we can see this is the fusion. Gene detection, you, can see all those blue, squares, indicate.
Those Samples, has, a particular. Fusion. Gene that's, diagnostic. Also. It's a driver events. And the, some of them can be actionable, for example. If. There is a. Fusion. Like, this. Ram, BP, to ELQ because, the algae is a tyrosine. Kinase. So, there's a drug directly, can targeted. This. Fusion. And. This. Part is summarized, or the DNA, seek and the RNA, sequencing. Of the, somatic, events. This, is driver, actionable. That's, including, all the mutations in those genes and, the. Little, plus signs indicated. This is a hotspot mutation. That means, it's. Recurring. And. It's proven, to be, disease-causing. Genes, are these disease-causing. Mutation. Event. This is the DNA. Copy number also. We. They're, validated. In the RNA, sequencing, make sure it's not only amplified, it, amplified. Also. They are overexpressed. So. This is the driver and actionable. And. Here, from the DNA sequencing, we can also identify the germline, mutation. And. Again. These plus signs are, these little plus, signs is a report. Germline. Mutation. That is now has no. Disease-causing. Function. Yeah. That's a. Yeah. That's a good question. Ended. Up, the. The director, answer, is. Not. Really, it's a little bit of hi slightly, higher in the in the pediatric, cancer but. It's not that, big. Difference, so currently. The detection, rate of germline mutation. In the cancer, patient is about the 10%, okay. Pediatric. Is a little bit higher but, 12% or so but. It's. Not. That dramatic. Again. Another, thing is. You. Know because. These are the pediatric, cancer they happen very early, on people. The hypothesis, is the most, of those patient, has drama mutation. That's. Reason they can have. No. Germ limitation. Yeah the reason we didn't detect these neither I. That's. My opinion is. Some. Mutation. We just don't know if, it is a disease causing a lot because, this German a mutation we only know again the, information of those. Mutation. Is, very, limited, and it's. Very hard to distinguish what. Is germline mutation, or private, mutation, you. Know by same, private, mutation, is if you just sequence, me, and you, everybody. Gonna, have thousands. Private snips. Which. Nobody has, in the whole wide world, okay. That's reason we can do. The forensic. Science, right you can make. Sure this is the Audion there's not other people's DNA but. Those, may be just normal snips, they're. Not disease-causing, but. Somewhere. And they indeed, a disease-causing. But. We do not know I. Just. Don't think we have a true, knowledge of disease-causing, rare and yet on the German German space. And. I. Want to highlight this. This. Part is, because. We. Can sequence, those, tumors. With. A very precision. Very. Very good precision, and we can immediately identify the. The. Diagnostic. Fusion. Genes for example there's, a four samples, I showed here, actually, the original diagnosis. Was not correct, is, it because we. Detected. Those are hallmark, fusions. And. The. Way were able to ReWalk. Revised, it at the time diagnosis. Of this tumors. And. This. Table shows, that, about the 10% of, those pediatric. Cancer. Patient we. Can detect the germline mutations.
And The, some of those are therapeutical. And. You. Know actually. This is a important. Thing because if this. Germline mutation, is detecting, a patient. It's. Not as. That. Means this German I'm a mutation. Might run in the family so. They have. A. Additional. Implication. For the clinical. Clinical. Meaning, for. The family not only for, the patient about the other also the phone for the family, so this is. Very. Challenging. Under other the ethical, thing. It's not very easy to deal with. This. This table, shows that about a 50%. We. Detect the. 30. Out of 59. Patient. We, can detect the actionable. Somatic. Mutation, okay. And, again. Some of you can see that, like the beer b-raf, mutation, 600. V600e. And the, we definitely, have the drugs against, the dose and the same with an elk. Ultimate. Ation and the, PTM, pi3k. CA. And. All. This, mutation, and. Potentially. Is. Actionable. So. In summary using. This technology, we. We. Demonstrate. The. Importance, and the feasibility. Of performing. This kind of multi-dimensional. Dynamic. In, the clinical setting in real-time and. A, 50%, of the children as. I told you has. Actionable. Somatic mutation, and a 10% have. Actionable, germ limitation. And the, important, the performing. The germ, lines. Sequencing. Is to. Find, the. Actionable. Therapeutic. Targets, for example DNA repair, genes. So. You can use. Use. The drug to targeted. This pathway. And the. Also. I didn't, show you the data but we also observed. That the increase the tumor burden in the relapsed tumor. That, the implication. Of. Using. Immune, therapy, for those. Relapse. The tumor because in, the pediatric tumor. The. Are the diagnosis, usually the mutation, burden is low but after, the relapse, the tumor, burden is higher so. Probably, we can use the immune therapy. To target, those new antigens. Okay. And the from, this study we envision, that the, Precision's. Therapy. For the fusion clinical, trial is. As following, so. If, there is a met hashtag disease, in. The current therapy. We, treat the others patient, in the same way okay. But. If we have a way to have. The use, the genomics, to. Detect, the biomarkers. We. Can sort them into different the categories, and some, patient if we know they have good signatures. And we. Can use standard. Therapy, to treat them and that they going to have better prognosis. But. For those. Poor. Signature, patients, and we, can further to. Detect, if they have a particular. Molecular. Events, that. Can use, as a target. Individualized. Comeback. Come. On combine, the therapies, to. Treat those patients to, improve their, survival. Rate and, those events can including, the, amplification. Of the genes mutation. Translocation. Over expression and, the alternative, splicing, genes or this, event can be, targeted. And. The. From the other study that we, now. We're. Building. Up this program, within. The CCR. Hopefully. We can offer. This, kind of service to. All the cancer patient in roading. The CCR, so, in, the city are the. Characteristic. Of the CCR cancer, patient is that they usually. Do. Not. Respond. To the standard, therapy so. They are referred to the and Nagy, and the CCR, to be, enrolled. On those clinical, trials to find. If there's any chance. They can be, responsive. So. When the patient comes to the CCR, and they can look in roading in different the clinical, protocol, and a, PRI. The. Principal. Investigator. They can all, this, next, generation sequencing, test. -. To. See what is the characteristic. Of the particular. Tumor, and all. These tissues, will, be procured, under go to the, LP. The. Laboratory. Of pathology. They, were do QC, and the nuclear, answer the extraction, and they're, going to send it to us, to. Perform the next generation, sequencing, experiment, and, the, data will, come out. The come, of this experiment. Is, German, and a the somatic, data and then we have genetic, border, or the tumor, board to, discuss what, is important. The change we detected, and those. Information. Were incorporated. In a clinical. Electronic. Medical, record, and to. Provide this information for. The pi2 you, use for the precision, therapy. Decision. And, another. Thing is all those data generated. That can be deposited into the b-trees system, which is an.
Edge. System. To. Treat. As a research, data and in the future we can mine those, data to. Have a new discoveries. So, that's the idea behind, this program. And. The. In this program, we offer both, exome. Sequencing. As a panel, sequencing, so, the exome, is we sequence, the other protein, coding genes and this. Is giving us the breadth, of this. The. Molecular. Profile, of a tumor, so. We can detect, the mutations. In dominant, close novel. Driver mutation, and the, actionable, secondary. Data for incidental. Findings, in the germline, in. In the non cancer genes and. The dis panel, we designed is to get the depth, because. The certain. Tumor, they might have clones. In the tumor, samples. If. We sequence like that the, the chrony fact it was deluded, in the tumor you we may, not be able to pick, it it up but. If we sequence. It very deep we can detect those event. So. And also this. Minor. Sequencing, also can validate, the, axon. Generation. Exome. Sequencing, and. Also. This one can provide, us copy, number change and age, the last. Loss. Of, heterozygosity. So. A lot of cancers, the, two hits will happen, is first, day lost the hetero zygosity and. Then being. Activated, another copy the other copy of the gene. And. Also, we can use this, for. The fusion detection. And. The. This. Program we also developed. A. Data. Portal, to, present the data you can imagine as I alluded. Earlier that. The genomic data it's. Not only, it's, a large quantity but it's very complex. So. We developed, this website. To. Enable, it, either physician. Doesn't, you don't need to, have. A, you. Know programming, skill to look into those data and the. You, know by the way you know those data is so big all the Excel, spreadsheet everything. We deal with in, text file you. Cannot, deal, with those kind of data you cannot even open those files you know so did so. To. Understand. And the to view those data can be very challenging, but. This kind of a way we can, host use, these website a host of data, and the we can builders. Date data very easily. Even. As, biologists. And. This, is the website and we can use. Energy. Credential. To log in and it's a secure data deposit. And it's access control, every time you log in you. Have a record, whose log in from where. And. We. Have a interact. Data viewing, so you can look at the QC of the data quality. Control, of the data and, you can look at the DNA sequencing, data the axon, cancer. Panel, and as well as the RNA sequencing, you can cross-check if, we I see the. Mutation, in the axon, DNA, data - is, this the same data in the cancer, panel or in, the RNA seek you can cross check all those experiment. And, there, is some screen capture, of that, for. Example this is a running, status. Statistics. This. Is a particular. Ripper represented. One sample when sequencing, and you. Can see this is all the total reads how, much we sequenced, and, what is the property. Of the sequence, are those, reads are unique, or there, are a lot of duplicates. And what's, the coverage. At the, 30, X, 50. X 100. X so on and so forth and also. We do genotyping. Using, those, genotyping. - to. Make sure if we say these, two sample from the same patient and the. Dish of the match genotype, like right. You. Know it's in the lab. It's very easy to swap sample, or make. Mistakes, and, that this is the two that we ensure that the sample, is the sample we think what. They are and. These. Are other QC. Tools we we have a circus, plot with, here we ploughed the. Variant. Allele frequency. In the sample, this, track is the germ land or the, green track this. Orange. Track is a tumor, you can see this, tumor, is the last has. A lot lost heterozygosity. In, the chromosome, 1 - this. Is the chromosome 4. And. They're also chromosome. 6 here, the this. Is an indication, of this is a pretty. Pure tumor, okay and here. Is the RNA coverage. And then, you can see this is a 5 prime UTR, all the way to 3 prime UTR so. The, coverage, is pretty even, if, you have a degraded, the RNA. You will say this curve, shifted, like this. Because. Every, time we're using the. 3-prime. Utr. Probe. To think sir sighs the, food. Clone and. The, diesel just, show the coverage, plot and this, is the hot spot coverage, or on those known.
Hotspot. Cancer. Cancer. Genes, what's the coverage, in that you can see it's, very high coverage in the panel, is about. 500. X coverage. And. This. Is a particularly. You for the mutation view and then, you list all the mutations and, there is all different annotations. From the public, database and, also. Give you the very. Early, frequency, you can see this, is a particular tumor, the. Real, new frequency, is less. Than on, the file most of them that, indication, there's a normal. Contamination. To this, sample, and. This. Is another view, of. Mutation. Will cross, all the patients, for, example. Here. On the top there's a lollipop, where. Shows that, the EGFR. Somatic. Mutation. Will detect the in the CCR, patient, and, the. Down here it's all, the mutations, detected in, does a large cohort, study, for, example the TCGA, or ICGC, study this, is like the aggregates, of hundreds. Of thousand, people or. Patients. The. Mutation, status for, this particular gene so this is a very important. Tool. For us immediately. We can realize, that for, example this one is a hotspot mutation. Because we detect. In. A lot of, patient. In those. Cohort, study. So. In conclusion I. Just show, you that the integrated, analysis. Of Cancer Genome identified. Biologically. Relevant diagnosis. Diagnostic. Prognostic, biomarkers, novel. Targets for the therapy, and those. Are powerful, emerging, tools, of. Sequencing, were, determined. Well. We're determined to complete the genome, portraits. Of a cancer at the, base pair, level so the other will increase. Our understanding, of the cancer, biology. Data, will also help, us to identify the, key, drivers, and being able to develop. The future novel, therapies, and. Again. This, is a teamwork. And the, is the involved, multiple. Different. The team from. Genetic. Branch from. Bioinformatics. Under. The, research protocol, is a clinical. Clinical. Supporting. Team and also. From the laboratory, of pathology. And. The. This. Are. All. This. Cleaning. Clean, omec, project. Is heading, by the palm. Roger which. Is the branch chief and, java. Calm as, deputy. Chief in, the genetics. Branch. So. I'm, going to stop here. If. You have questions. Yeah. That's a very good question you know for. The diagnosis.
Samples. Indeed. That is the case but, the as the odd or data. And other people, study when. To relapse, usually. The, mutation. Burden increase, dramatically. You know. Three. Times even sometimes, to ten times so, in, that case you still maybe. Have the chance to. Invoke. The immune response from. You, know this. Check. Checkpoint, inhibitor, so. But but this is a research. Activity research. Field. Yeah. Yes. Oh. Currently. For. The whole exome, we, we report, about. 10%. Allele. Frequency, but for the panel we can go to 5%, as a, matter of fact we can determine. Detect. The lower frequency. But. We. Have a we. In order to have, enough. Sensitivity. And the specificity we. Choose 10%, of 5% actually we can go down, even lower. Okay. Okay. Thank you. So. We have a few announcements, one. Being that, June. Will be leading, the genomics. Court or on Thursday. At 3:00 and, many of you have signed up for that so. You go, over to building, 37, the. Second. Floor I'll be sending you an email to remind you on Thursday. Okay. So it's the vestibule, by the South elevator. And. The. Second. Announcement is next, week, Traco. Will be on Tuesday not Monday and. Then. Unfortunately our, other speaker, today. Was. Not, able to be here so, through the miracle, of modern, technology we're. Going to be showing you the talk from last year so. My name is Karen Dunleavy and I'm the. Clinical director of the lymphoid malignancies, branch at the National Cancer Institute, and over. The next 45, minutes or so I'm going to talk about, lymphomas. The. First half. Of the talk is some general principles. About, the biology, and, treatment. Of lymphomas, and then I'm. Going to talk about some of the research. That we have been doing in. Our branch just to give. You some sense of the translational. Work that we can do in lymphoid, malignancies, here. At the NCI. So, in terms of how common lymphomas, are compared. To other. Cancers in the u.s. in. Males. They're, the fifth. Most common cancer, type and in. Females, they're the sixth most common cancer type. But. The incidence of lymphoma, is increasing, and. There are a lot of reasons for that. First. Reason is probably because there, is an, increase in the elderly population so. As. With really all cancers, as people get older they have a higher chance of, developing cancer and, that's, true for lymphomas. Particularly, for certain. Subtypes of lymphomas. Also. Certain. Diseases. Are associated with lymphomas, HIV, is associated. With it if you're hiv-positive you've, got a better 100. Times increased chance of getting the, most common type of lymphoma which is called a few large b-cell lymphoma and, about a thousand times more increased. Chance of getting Burkitt lymphoma which is a pretty rare lymphoma but it's, often. EBV, driven, and strongly. Associated, with, HIV. And. When, we talk about lymphomas, there are Hodgkin. Lymphoma and, non-hodgkin. Lymphomas, and, as you can see in, articles the films are much more common they make up 83 percent of all in farmers and Hodgkin. Lymphoma makes, up 17%. So. In. The u.s.. I'll. Focus on non-hodgkin, lymphoma a lot during this lecture there, are 75 thousand, cases. Of non-hodgkin, lymphoma per year, and. As I said the. Incidence rises with age and that's the biggest reason why we're seeing an increased incidence. Of lymphomas. And. Shown here are, seer. Data. Showing. You the period from 1992, to 2010. And the, incidence, of NHL, in both, males, and. Females. And. As. You can see there there has been an increase in the, incidence, of NHL. In. Both males and females during, that period of time but. The good news is that there has been a reduction, in, death rate from lymphoma during. That same period of time in both, males. And females. As. You can see from these curves. So. For, for. Most people who develop lymphoma, there is no, known, easier, logic factor. But. There are certain. Factors. That put. You at increased risk, of developing lymphoma. So, people, who've got altered immunity, have got an increased risk of lymphoma, some.
Of The examples, of that are. Diseases. Where you have inherited, altered. Immunity, like wiskott-aldrich. Syndrome as, I. Said. Acquired. Altered, immunity, patients. Who, have HIV have got a much increased risk, of developing lymphoma. People. Who who have iatrogenic altered, immunity, such, as people who have undergone a. Cardiac. Transplant, or renal transplant, or bone marrow transplant, either on immunosuppressive. Drugs, these. Patients, have an increased risk of developing on farmers and they have. A particular type of lymphoma, called PTL d or post transplant, lymphoproliferative. Disorder. And. People who have had certain types of chemotherapy are, also at increased risk of developing lymphoma. At. The nih we have. A group who study, Sjogren's, syndrome and, interestingly. When, we do the, blind. Biopsies, of these patients you could do blind lip biopsies, and you find that. Almost. All of these patients have got, out. I've. Got evidence of. Mucosal. Associated lymphoid. When. You look for it so I'm autoimmune. Stimulation. Is. An. Increased risk for a lymphoma. Acquired. Immune stimulation, is. Helicobacter. Pylori, is an organism which you can get in the stomach and, there. Are certain lymphomas, in the stomach that are associated with this and actually. In. Some cases if you eradicate the, organism, if you eradicate Helicobacter. Pylori you can see regression, of the lymphoma. That's not in most cases but it's in some cases, I'd, have a tie to see an HIV are also examples. Of this. Our. Understanding, of the link between chemical. Exposure, and, lymphoma. Is. Not. Not very well-established. But. It would appear that certain. Chemicals like organic, solvents. Agricultural. Chemicals, and maybe others are associated, with. Lymphoma. There's. A lot of interest at the moment in the. Microbiome, and microbial, oncology, and. What. We've certainly identified, some organisms, that are definitely, linked, to lymphoma I think there are a lot of other. Infections, that. Possibly. Cause lymphoma, but this, has not been definitively. Established. At this point in time so. Of. The, infectious. Ideologies that have. Been. Associated. With various lymphomas. Burkitt. Lymphoma as I said is a rare lymphoma you see three different types of this you. See endemic, Burkitt lymphoma in. Regions. Of the world like Equatorial. Africa. It. Usually occurs in children. Between. The ages of 3. & 5 and this. Type of lymphoma might often presents with jaw masses, and it is linked to EBV in. 100%. Of cases the. Other two types of Burkitt lymphoma are. Sporadic. Burkitt, lymphoma which is the type that we see most commonly in the US and then hiv-associated, Burkitt, lymphoma and both sporadic. And hiv-associated, Burkitt, lymphoma. Are. EBV, positive in about 40 percent of cases. Hodgkin. Lymphoma can, be linked to EBV, and post-transplant lymphoproliferative. Disorder. Particularly. After a kidney transplants, and heart transplants, can be linked to EBV. Obviously. AIDS related NHL, is linked to HIV. There's. A unusual. Leukemia, lymphoma called. Adult, t-cell, leukemia lymphoma. Which, is caused. By the htlv1. Virus and, this. Again is seen in, distinct. Regions of the world, in the Caribbean. And. These, patients develop, atll. Which is a very aggressive lymphoma and, is largely, incurable. And.
Most Of the therapies that we use for other lymphomas, don't work for this type of lymphoma. Primary. Effusion lymphoma is. Seen. Almost exclusively, in patients who have HIV and it is linked to the hhv-8. Virus. As. Is, multiple myeloma, lymphoma. Plasma silica lymphoma is linked to hepatitis C I talked about molt linked to Helicobacter, pylori. And. Mediterranean. Lymphoma. Is linked to an intestinal, pathogen. So. The. Most important thing when, a patient has lymphoma as newly diagnosed lymphoma the most important thing is the pathology. And getting the pathology right and. Really. The tissue needs to be looked at by a, pathologist, who's really expert, in a matter pathology, and in looking at lymphomas, and has, seen. Lots and lots of these lymphomas. Before, because. They're. Becoming here they are a very complicated group of diseases, so. I think it's best if the person. Making the diagnosis, is, not a general. Pathologist. Who looks. At all different types of cancers, but it really focuses, on lymphomas. And. Heat. Hematological. Diseases. And. The. For. All cancers, there's a w-h-o. Manual. Which is, very, helpful in making the diagnosis, for pathologists, and it really. Lists, all the different types of lymphomas, and their. Different characteristics, under the microscope, and also, clinically. How they how they present and. Were. Certainly. In an era now where a. Lot of lymphomas. Should. Not only be diagnosed, by how they look under the microscope but also how the patient, presents so, this. Is called a clinical pathologic. Diagnosis, when we have, a new patient with lymphoma and we look at their biopsy, with our, pathologists, they always like to know about, how. Older this patient, what, did they present, with what did their CT scan looked like. So. It's. Important. For them to know that because that helps in both. Establishing. The diagnosis, and in doing, that they can they, can request special, tests on the tissue that will. Be. Guided by the clinical presentation. And. Then lymphomas, are classified, according to whether, their, t-cell, or B cell about, 85% of lymphomas are b-cell 15%, or t-cell. Their. Location, in the lymph node. The. Appearance of the cells. Molecular. Features. Specific. Genetic abnormalities. And. Clinical. Features what. The history was coming, in and what disease sites the patient has. And. If you look at the breakdown of non-hodgkin, lymphoma the most common type by far is diffuse large b-cell lymphoma, that makes up about forty or forty-five percent followed. By follicular, lymphoma and. After. That there are a number of different. Types, but they're really, pretty rare as you can see here, so. For the most part when we have lymphoma patients, they have diffuse. Large b-cell lymphoma, or, follicular. Lymphoma. As. Shown here is the lymph node and depending. On, where. In the lymph node the lymphoma. Arises, from it can be very very different. For. Example you can have marginal, zone lymphomas. Which. Arise, in the marginal, zone and follicular. Lymphoma which, obviously arise in follicles. So. This is. Important. For the. Diagnosis. And, most lymphomas. Are b-cell. Lymphomas. And. You. Can. Correspond. B-cell lymphoma with the different stages of b-cell differentiation. So. Precursor. B lymphoblastic. Lymphoma ways you. Can correspond that to very early b-cells, I see a little a little bit later and then, the, main. Lymphomas, that we see a little, bit later and I'll talk I'll talk. A little bit, about this in relation to the few Sarge be so far because that's the most common the common astrology. And when the pathologist is, looking at a. New. Lymphoma under, the microscope they. Use.
Immunohistochemistry. To. Decide. What type of lymphoma it is the lymphoma has a particular, appearance in terms of its morphology. With. H&E but, immunohistochemistry. Is very helpful this was something that really wasn't around 20 years ago so. For. Example if they if it looks like it if you start b-cell, lymphoma you would do, cd20. Bcl6, mum, 1c, d-10 and all of these stains will be very helpful in. Telling. You that that, is the definitive diagnosis, and likewise there are t-cell markers, which can tell you it's a t-cell lymphoma so, immune as the chemistry is very important. Cytogenetics. Are done in certain, in, certain cases, for. A. Lot of b-cell, lymphomas, follicular, lymphoma and, a few started to be so infantile they have frequently, have a 1418, translocation. Leading to over. Expression of bcl-2, so. That's, found. In close. To a hundred percent of, follicular, lymphoma and, in about. A third, of diffuse. Large b-cell lymphomas. The. Lymphomas, that are associated with Helicobacter a lot of those can, have, an 11 18 translocation. So if, the pathologist, is told this lymphomas coming from the stomach that's something that they might do to confirm that it's a, Malter. Mucosal, associated lymphoid tissue, lymphoma, and. Burkitt. Lymphoma has, a, Mik. Rearrangement. So that's a an 814, translocation. That's present at 100% of. Burkitt. Lymphoma so, Burkitt. Lymphoma is a very easy, lymphoma. To diagnose, under the microscope, it's got a particular, what's. Called a starry sky appearance. Because. Of the high, proliferation. Of the tumor cells but if you. Check. For a Mik, rearrangement. It's positive and hundred percent of cases there's. An unusual, type of t-cell lymphoma called, and a plastic large, cell lymphoma and that's got a two-five, rearrangement. So. The pathologist, really decides. To. Do these tests BAE on their. Suspicion. Or where, they're going with the diagnosis, they're not done on every single lymphoma, it's. It's really guided by how. It looks under the microscope. So. Then when. You have a patient with newly diagnosed lymphoma how do you evaluate them.
The. First thing is you ask them what has been going on with them. What. Have they presented. With. The. Most common. Presentation and. In, lymphoma, is having lymph adenopathy and, people usually notice this. In. Areas. Where you can feel your lymph nodes so they notice that in their neck under, their arms in their, groins, if. You have lymph. Nodes in your abdomen, it really takes a long time before you notice them so most. Of our patients when we ask them what. Have you been complaining of they usually say I noticed a limp in my neck or under my arm or in my, groin and. And. These are usually caused by infection, but, when. These are caused by lymphoma they're I mean they usually don't go away without the biotics obviously, and they're, also usually non-tender, infectious, lumps tend to be tender. Whereas. Most patients who present with lymphoma if they have a lump they'll tell you that it doesn't hurt at all and it. Isn't pretty causing me any discomfort, or any distress. In. The history we all we, are specific, questions about you know how, people have been obviously, but there are symptoms. Called be symptoms, and, those. Are fevers, night sweats, weight, loss of more than 10% and those. Are important, because they, put. Patients, in two different prognostic. Categories, so depending. On the lymphoma type you come in with if you have these symptoms that might, indicate that you have a more, aggressive lymphoma. And, it's, associated with it with the worst prognosis than, if you don't have these symptoms. Everybody. Who. Comes in you should you, should examine them obviously that's. Very important, and then do blood, tests. All, of the basic tests should be done, there's. A test called lactate, dehydrogenase, which. Is. A liver enzyme, but it's a, nonspecific. Test, of tumor, and that's often, elevated, in aggressive, lymphoma so that's a test that patients. Should have done once. All the and. Everybody, with who presents with lymphoma they, should have a HIV. Test done. Because. Of the association. With. HIV, and they should also have hepatitis screening, done, they. Should have hepatitis screening done for two reasons one, being. That hepatitis can, be associated with lymphomas, unto certain. Types of hepatitis can. Reactivate, with, chemotherapy and, with rituximab which is a drug that. Nowadays. We give to all patients with b-cell, lymphomas. Everybody. Should have imaging, of. Their chest abdomen, and pelvis and, that's called staging, and there.
Are Four different stages, stage 1 2 3 & 4 and stage. 1, or 2 disease means, that the disease. Is on one side of the diaphragm and if it's 3, or 4 it's on both sides of the diaphragm and. That's. Really. Becoming less important. 20. Years ago was important, because of people that very early stage of the disease they, typically. Got chemotherapy. But then they got radiation treatment, if it was in one particular. Location but, nowadays. Radiation. Is used less and less frequently, so, staging. May be becoming. Less. Important. Almost. All patients should have a bone marrow aspirate, a biopsy done in. The b-cell lymphoma is the most common ones and follicular, lymphoma the. Bone marrow is involved in a very high percentage of cases probably, about 15 to 20 percent of cases of diffuse large b-cell lymphoma, and. And. Then, other studies, should be done as indicated, there's. A lot of work, in looking at the role of, fdg-pet. Scans, and the initial diagnosis, of lymphoma so, a lot of doctors will do these, and. Then, depending, on where the lymphoma presents, for. Example if you have a lymphoma on your brain, it's. Best, to do an MRI scan, and certain, types. Of lymphomas, in certain presentations, should have their. Spinal, fluid checked so, if. You, have aggressive b-cell, lymphoma and if you have involvement, of what. Are called extra, nodal sites. It's that are, outside. The lymph nodes or. If. You have involved, with the bones or if you have a very high LDH, level, there are certain criteria that. Suggest. That it's really important to check the CSF, because the, treatment that we give to patients it. Doesn't really get into the central nervous system, it doesn't for the most part penetrate, the blood-brain barrier so, you, really want to know if a patient has involvement, of the spinal. Fluid it's it's rare to have it but it's associated, with certain clinical factors, so if a patient has those then we, would recommend that you check the CSF, and. You. Know it's fine to interrupt me at any point if you have any questions but just are, we. Gonna ask we I'm happy to answer questions at the end. This. Is the staging system that I told you about I won't go into it too much but there are four different stages, and one, being just one lymph, node area and for being diffuse, or, disseminated, their involvement and, involvement, of external, sites and. As. I said the morphology of lymphoma, is important, this is a diffuse, large b-cell lymphoma. Morphology. And. Typically. You, see large cells they're about twice, the normal size of, a lymphocyte. They. Have vesicular, nuclei, prominent. Nucleoli, and are basal philic, and they're large. Cleaved or multi located cells and. They. May be rich in T lymphocytes, so. Over. Recent. Years there's been a huge. Amount of interest in in in the tumor microenvironment it. Might be something that some of you are are, focusing. On but it's really important, in certain. Types of lymphomas so not just the tumor cells but the the. Infiltrating. Immune cells around the tumor cells and in. In. Follicular, lymphoma and a few Sarj b-cell, lymphoma if, you look closely at what these infiltrating, cells are and what their genetic. Expression, is you can, predict. How certain patients, will do so the. Tumor microenvironment is, becoming very important, in lymphomas, and we're starting to develop therapies, that, actually, target, the microenvironment not just the tumor sells but, also the microenvironment. Okay. So what about, the. Outcome, of patients with, lymphoma how, do they do or most. Of them cured. And, for. This talk I'll just I'll focus. On diffuse large b-cell and found with quite a bit because that's the most common. Type and the type that you, see, the most when you look after patients with lymphoma so. These. Are coupling markers. Then they show on top, overall. Survival and, progression-free. Survival on. The bottom and. You. Can see here that the interval, is in months so this. Is that - a hundred months which is quite a long time. And. These. Are patients who of, all ages who had if you start to be selling FOMA and they received, the. Standard, treatment, which is a, chemotherapy. Regimen, called chop which is. Cyclophosphamide. HS. Hydroxy, donor river son or doxorubicin. O is on, kovin which is the trade name for vincristine and P is prednisone which is a steroid so, an or, is rituximab, and, over. The past 20, or 25, years the most significant, advancement.
In Treating, patients with DLBCL. Has. Been the addition of her Texan lab to chop chemotherapy. That. Has increased the cure rate by. About. 10 to 15 percent so, it's very important to give her Texan mabh and. It's. Interesting because the, the adult, world and the pediatric world in lymphoma are very separate, and. The. Pediatric world has been very hesitant to give vertex mode but they really haven't been giving it to. Everybody up until a few months ago where they were doing a big randomized. Study in children and they were randomized, to get rituximab. Or not to get vertex mode but they have. Recently shown, a. Little, bit earlier than they expected, that there. Was a significant, survival advantage to giving rituximab, so. Now everybody, adult, and child who has a few, Sarge b-cell lymphoma gets, rituximab. But. I think what these curves tell you I mean if you're a new patient with, DLBCL. And. These, are. Patients. Can be divided in two. Lower-risk, IPI intermediate. Risk or intermediate, high risk IPA it's called the international prognostic, index and it looks at. Your. Age the, stage of disease that you have whether, you have an elevated LDH. Your. Econ performance, status so if somebody's really, fit at zero if somebody's not really fit and lying in bed it's 2:00 to 3:00 and then, the presence of extra nodal sites and that's what the low risk intermediate risk and, high risk is but these, curves just tell you that with standard treatments so all around the world if you go into. An oncologist, with diffuse, large b-cell lymphoma when you get our chart but you can see that for. A. Significant, proportion of patients standard, therapies not adequate, so you. Know while most people have a long overall, survival, a. Lot. Of people don't and a, lot of people progress as you can see from the curve on. The bottom. So. Our field has really been trying to improve the cure rate for DLBCL. And. A. Lot, of a lot of different strategies, have, been tried, what. Have people been doing you. Know they have said well we usually give six cycles of workshops, so let's, try giving eight cycles see how that works and that has not been helpful, it's. Associated with more toxicity, but no increased, benefit, they've. Tried therapy intensification. So. Arch up is typically, given every 21 days so. People have tried giving it every 14, days in Germany. About ten years ago there. Were some studies that suggested, that if you gave it more intensely, it, was associated with a better outcome but about a year ago a group, in France and a group in the UK did large studies, of patients where they gave. Half the patients, or chopped every. 21 days and half the patients are chopped every 14 days and there was no difference in both studies and the patients. Who got it every 14 days actually had more toxicity, so that, wasn't helpful. People. Have tried doing bone marrow transplants. When patients, go into remission, that's. Not. Been of any benefit. That. They've tried giving maintenance, rituximab, that's where people finish their rituximab. A chav treatment, and then they continue. To receive. Protects in lab for 18, months or 2 years after, that and. Studies. Have you, know again half the patients have had, maintenance rituximab, half had not had not and, there, was no difference between the two groups.
What. Are promising, strategies. Well. Are there better chemotherapy, platforms, in our chopped. The. The French developed a regimen. Called or a CV BP and in in young. Patients, who, have a low ipi, score. That. Was better than our chopped but i was a very small proportion of patients who get DLBCL. And. Our. Group has been doing a lot of work with doe, suggested, epoch or and we're awaiting the results of a a randomized. Study. We. Have a lot of novel agents that are based on the. Identification, of new pathways, in different, types of lymphomas, and I'll talk about those a little bit but I think that that probably offers. The most promise, for improving curate. Is to, incorporate. Some of these effective, novel agents into. Up. Front standard regimens, like our chopped, but. You know as in our field it's really critical, to develop, novel, agents that and approaches, in the context, of bio the, biologic, subtypes, and factors. So. In that respect. Historically. We always thought that DLBCL, was, one disease that it, was just one entity and. This. Is work that was done by the. Lymphoma and leukemia molecular. Profiling, project is but it's a it's a big project that involves a lot of institutions around, the US and Canada and it, was led actually by loose, stats lab which. Is based at NCI and about. 20 years ago they. Applied. Gene expression, profiling, two. Cases. Of lymphoma,
2017-11-25 01:40


