Suicide Prevention What You Need to Know
Hello. Everyone, this is Matt. Gilbert I made licensed, Marriage and Family Therapist. And certified. Employee, Assistance professional. For your Washington, State Employee. Assistance Program. I am, honored to be joined here today by, a. Colleague, of mine dr.. David. Luxton, dr.. Luxton, is a, nationally, recognized, expert and, trainer in suicide, prevention, telehealth. And innovative, technologies, in behavioral, health care. Dr.. Luxton is a founder and CEO of Luxton, labs LLC. Chief science officer, now, matters, now. Thorgy. An, associate. Professor in the department, of psychiatry and. Behavioral, sciences, at, the University, of Washington School of Medicine in Seattle, dr.. Dr. Luxton rather previously, served as a research health scientist, at the Naval Health Research Center in, San Diego California where, he, served as the principal investigator of, the Millennium, Cohort. Study. The. Largest perspective. Health Study in US, military history. Before. Moving to San Diego, he served as a research psychologist, and. Program, manager at the National Center for telehealth and technology, with. A defense health agency a, Joint, Base lewis-mcchord, a seasoned. Researcher, he has authored more than 75. Scientific. Articles and book chapters and, published. Two books artificial. Intelligence, and behavioral, mental health care in, 2015. As, well as a practitioners. Guide to tell him mental, health in, 2016. He. Has also helped to develop national, guidelines for telemental, health and, clinical best practices, in the use of technology, and behavioral, health care in. 2015. Dr., Luxton was awarded. The American, Psychological Association. Division, by teen or military psychology, the, author W Milton award for early career achievement. Dr.. Luxton is a licensed, clinical psychologist. Musician. And a veteran of the United States Air Force it is. With great honor and privilege that I'd like to welcome dr.. Luxan. To our first, ever webinar, on, vital. Suicide, prevention. What you need to know without further ado here is dr., David Lester. Thanks. Matt. Good. Afternoon everyone. It's. My pleasure to be giving this presentation today it's, a very important, topic as. We get going here if at any point you have trouble hearing me please, send, the text, Matt, and I are kind. Of tag teaming the screens here so he's going to be checking the messages, while, I'm going through the presentation.
Okay. So we have some learning objectives for today. This. Is a one-hour presentation this, could easily be a couple hours, however, I've condensed, it down into, one hour really just sort of need-to-know information, this. Information is, geared towards both the individual. Who. May. Know someone who is in crisis, or thinking about suicide or having suicidal thoughts. Individuals. Themselves who may be having these thoughts but also for managers. Persons. Who may. Have supervised these that are in crises and I'll give you some tips for working in those situations. To. Get started we're going to talk about, suicide. Risk factors, and statistics. Regarding the risk I think this is important, because it really paints the picture of. The problem but it also tells us a lot about the. Risk factors things to be looking out for it, you're. Going to become knowledgeable of how to talk to employees co-workers, friends and loved ones who may be in crisis, and to commit suicide. I'm. Gonna provide some recommendations, for coping with a suicide, loss or attempt and. You're gonna become familiar, with available, prevention, and support, resources that, are available to you. First. Off preventing. Suicide, is everyone's. Business and, what that means is that we, all can and should play a role in preventing, suicide. Prevention is not just in the realm of health care providers we can all do something to, prevent, suicide. Started let's talk about some of the myths and facts about suicide, and self-directed violence, what I want to do here is kind of test your knowledge so. As I go through these, you're. Welcome to. Text. In what you think the answer is or you can just stand by kind of think about it and I'm. Going to test your assumptions. Okay. Talking. To a person about suicide, can give them ideas or, be interpreted, as encouragement. True. Or false. Okay. See. People coming in saying false, well, those people all, right, evidence. Shows that talking, about it does not encourage, suicidal, behavior, it, can instead provide persons, with options for seeking help and making safety plans. How. About this one only, people with psychiatric disorders. Are suicidal. The. Correct answer is false many, people coping with mental disorders are not suicidal. And not all people who take their lies have, a diagnosed, psychiatric. Disorder. Majority. Of suicides occur, without learning, signs true or false I. See. More people entering, in false their. Correct majority, are preceded, by warning, signs some. Estimates indicate that about 8 out of 10 suicides. Are. Indicated. With some kind of warning sign and these include both verbal and behavioral signs and, some suicides, will ever occur, without one. About. This one a person. Who is suicidal is, determined, to die. Okay. It's false suicidal. Persons, are often ambivalent, about living, or dying. How. About this once. A person is suicidal, they will always remain suicidal. Or high-risk. False. Heightened. Risk is often short-term, in situational, suicidal. Thoughts are not permanent. How. About this once an emotional state improves, the risk for suicide, is gone. That's. False the highest rates of suicide occur, within three months an improvement in depressed state this. Is can also be related to. Antidepressant. Medications, where they, often have warnings about suicide. Risk while, one of the reasons for that is, basically what this fact. Is about that. When people are alleviated from depressed. Feelings. They can actually can, actually increase the risk for suicide, if throw a high risk a.
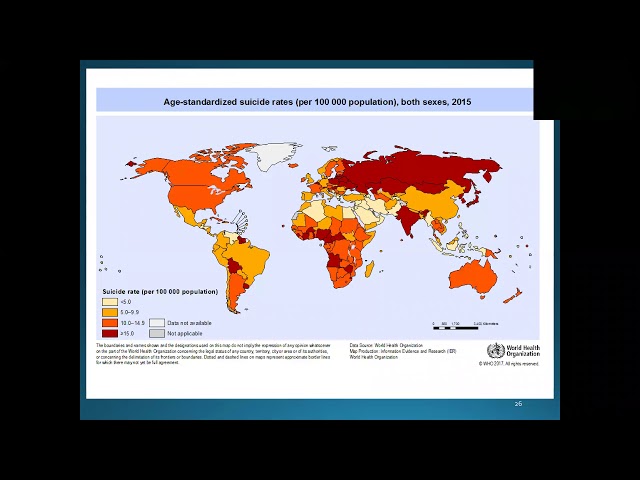
Person. Who attempts, when non-lethal method, is not serious, about God. That. Is false many, people attempt prior to completing suicide, and they, may in a sense be testing the waters. Or. Suicides. Occur doing during the holidays. That's. False according. To the CDC, the Centers for Disease Disease. Control, november/december, actually have the fewest suicides, now. Does that mean that for some people, seasonal. Effects. Around. The holidays etc, can increase, depression, but, statistics, show that in itself is not enough. All. Right so now let's see if to talk a little bit about definitions, and I'd like to present this because we. Often have misunderstandings. About. Suicide. Is definition, and how the terminology, is used so these these. Terms are coming from, Disney's, control these are there there's an armature that's been published. Self, directed violence this is the same thing as self interest behavior, this behavior that is self directed and deliberately, results, in injury or the potential to injure oneself so. It's key about this is they're really two types there's. Non-suicidal, self. Directed violence so, this is when people do some kind of self-harm behavior, but, there is no evidence whether implicit or explicit that. They want to die by suicide in. Their, suicidal, self, direct violence this is when people. Engage a self-directed, violence. But there is some kind of evidence either implicit or explicit that. They, have intent to die. Suicide. Is of course death caused by self-directed, interest behavior with an intent to die as. A result of behavior, suicide. Attempt is a non-fatal, self directed potentially. Interest behavior, women tend to die as a result of the behavior but it might not result in injury and of, course suicidal ideation, is they're thinking about or considering, they're planning suicide. So. The terms committed, suicide, and completed says these, are used all the times by the media. What. I hate even more than those terms are successful, suicide these terms are discouraged. The. Field really, does not use these or should not use these preferred. Terms are no presently death by suicide or, died, by suicide. Suicide. In itself is not a crime in this country I just have a history, of me considered a crime and, so it's not like you're committing, a felony, you. Are dying by suicide. Alright. So now let's get into talking, about some of the need-to-know statistics. Regarding suicide, and, self-directed violence, now my intent here is not to bore you with a bunch of statistics, I want, to point out what I think are the most important, things that you need to know I will, go through these relatively. Quickly but. If you do have any questions about any, statistics, or really anything else that I talked. About today during the presentation, feel, free to enter those into your chat I certainly. Do more chat at the end I will leave a few minutes for some additional questions. Alright. So this data is from the CDC, and this is the most recent data available and. What it is showing is, rates. Of suicide among, age groups, here, in United States. Suicide, is indicated, by the green, squares there and, as you can see in just about, every age group from, age 10 up, suicide. Is in the top 10 causes of death what's, most important, to me is, that it's the number two cause of death between. Ages 10 and 34. And. As you can see that that risk is, still extremely high lives, throughout the life. Here's. The graph showing it worldwide, this. Data is for, mixing, data from different countries, about high-income and low-income and, middle-income countries, I don't, really know that what. The cutoff is for income, here but just, just sort of how the World Health Organization, classifies it. As you. Can see that the. Rates of suicide are, much higher among younger persons. And. Much, higher in, countries with lower middle income. Now. In this and you might be wondering well why is that well. One reason is, just the availability of resources so. In higher, income countries. Are hiring from families they have more access to resources, mental. Health care et cetera. Now. This next slide kind. Of shows the, rates of suicide throughout, the world this, is 2015 data, it. Is adjusted. For age because I will, show you here in the, forthcoming slides, you'll, see that suicide. Rates differ by age and, they.
Have To make it statistical, adjustments, to equalize, things when, comparing different groups or populations, as. You can see here the, United States is, between. 10 and 14 point 9 per. 100,000. Deaths. And. Other. Countries in the world such as the. Former. Soviet Union and some other areas in, Asia. And. In Africa and, a couple places in South America, very. High rates greater, than 50 per 100,000. Again. I can't say, exactly why, that is probably. Back to the same point, about the availability of resources, that. Can also be some other cultural reasons, but it's primarily the ability, of resources. So. In the United States the, annual. Age, adjusted suicide. Rate is thirteen. Point two six, per 100,000. So, about the total number of deaths in 2016, or about 44,000. So. On average here in the US there are about 118. Suicides, per day. There. Are more than twice as many suicides, in the US and where homicides, that doesn't. Get your attention I'm not sure it will. Approximately. 1.3, million persons, in us make non-fatal attempts, every year. Now. This slide is showing the trend across time since 1999. There's. Been a 24%. Increase, in. Suicide. Rate since 1999. It's. Really been increases for both men and women really in all age groups between, 10 to 74. However, the percent increase in suicide rates for, women. Was greatest for those younger. Women 10. To 14 years old, for. Males those age range increased. Between 45, and 64, and there's, been discussion, of literature and Studies on why it's increasing, for young for girls and adolescents. One. Theory that's been kind of thrown around is the role of social media and, how that impacts, young. People in particular and, there's been a number of studies shows from this there I cannot, say that that is the cause of this trend is. Probably, as. Some researchers showing, a factoring them. Here's. A slide that comes. From the American Foundation for Suicide Prevention and this one here is showing specifically. Data for here in Washington, and. As you can see suicide. Is the eighth leading cause of death overall here in Washington, and our. Rate per, 100,000. Fifteen point three seven, and we're, just higher than the national average and so. This certainly. Is something that gets my attention and. As. A health care provider and, a, public, health professional I don't often think about things, as terms as money, like how much suicide, cost here in Washington, but health. Economists certainly, do this and, as you can see we're time a billions of dollars in, combined lifetime, medical on work loss. At about one point one six million. Cost. Dollars, per. Suicide, death so the impact of suicide. In. Itself in some incredible. But also, its impact on. Society. As, far as like lost employment, etc is, huge. So. There's a little bit more statistics, here in the, United. States firearm. Suicides is. Really number one as. Far as cause of death number. Of deaths is just over twenty one thousand, six. Point seven per 100,000. People firms. Account for fifty, one percent of all suicides here, in the United States. Suffocation. Is the second most common and. There's. About eleven, thousand, per year that's. By suffocation. Poisoning. Third. With, about 6,800 per year although. There is include things such as Falls drowning, and trending appear state, and. I am going to talk a little bit more here in a moment about farms, who is died in prevention. So. Here's some statistics on, dinner. Differences, in suicide, so men die by suicide three, point five times more often than women - in the US women. Are more likely to attempt suicide however. White. Men account for seven out of ten suicides, as, 2015, data the. Rate of suicide is, highest in middle-aged men and. The. Rate among 4506. Referrals is 19.6%. Sits. Really the highest age. Group, in. A gender as. Far as suicide. Men. Are more likely to use their methods. Such. As firearms or suffocation, however, women, are more likely than men to attempt, suicide by, policemen. There's. Differences in race and ethnic groups as well American. Indians and Alaska Alaska, Natives, have the highest rate of suicides, followed, by non-hispanic.
Whites, Hispanics. African. Americans and Asian Pacific Islanders, each a suicide rates are about half their lives in American Indian Alaskan native counterparts and, this is data coming from the nationalist mental health. These. Next two slides show it by occupational. Group this. Was. Published in a paper that's published through, the CDC it's, pretty recent data I thought, it's, quite interesting as. You can see here the number one group occupational. Group with the highest suicide rates, is. From farming. Fishing and forestry and. Interesting. League here in Washington, you, may have heard that there was a bill put. Forward by. Congress. Person oh look ox related. To, focusing. Suicide prevention among really, this kind of group or farming, and it's. Really based on this data it's, very high here in Washington. And. As you can kind of look at the slide you can see how it's different across different, groups. You will notice that there is a definitely, a gender effect, here you, can fact in the first the top three, farming. Fishing forestry, as well as construction and micro, maintenance repair. Professions. They're only including, data from in here because their women, are less representative, those in. Those career fields but, you can see that those rates are extremely high. In. Those, professions. This. Is important again because we can target, interventions, in different ways towards, these different, groups, here's. The second slide related to occupational, group. See. How that kind of reduces. In, some other professions. You know when I look at this heart do I see trends, in this some. Ways like I'm glad to see that health care and community, social service they're lower or closer, to the national average. Which. We think well maybe these people know, about resources, and they're able to get them, but. I do think this is important information to observe. Okay. So self-directed, violence among children. Adolescents and, young adults it's, the third leading cause of death for young people between, ages 10 and 20 for lifetime. Prevalence here in the US for attempt, is about 4% by. The way this is data is coming from a publication, by kinematic, and colleagues in 2016. 50. To 100, suicide attempts for every completed, service, Madol essence the. Rate has doubled in, the last 50 years which, is quite alarming it, does vary by sex and age it's, greater in high school girls versus boys 21. And 31% verses 13, to, 20. Percent of boys. Adolescent. Boys however are more likely to complete suicide, than, girls. There's. Just a quick slide showing, suicides.
And Jails and prisons. It. Is really the second leading cause of death in, jail, or in prison and, it's. Quite high to get something like on average. Between. 50, and 60, per 100,000. So. It's a significant, problem in, those, kinds of cities. And. This is a slide, showing rates among veterans this one hits, me personally as a veteran myself and, having worked in military, suicide, prevention for many years, the. Annual suicide, rate is 29, point 5 or 100,000. Veterans. Roughly. 50% higher than the rate among comparable. Civilians. That's. Way too high, in. 2014. An average of 20 veterans died from suicide each day 6. Of the, 20 were users of VA services, in. 2014. Approximately, 65. Percent of all veterans who died from suicide or, aged 50, years or older and. After adjusting for differences in age risk, for suicide, was 18% higher among male veterans for comparing US civilian, adult males after. Adjusting for differences in age risk, for suicide, was 2.4. Times higher among female, veterans when, compared to us playing at all females. So. On this next slide I'm going to show you kind of the rates. Across. The United States based on state data. And. As you can see Washington is up in that higher group, among. Deaths among, veterans, by. Suicide at 25 percent to 28 almost 27. Percent so. It's quite high here, do. I have an answer for that I. Don't I mean, there's a lot of veterans, who retire here a lot of military service members here as are on other states but. I did not have an explanation for. One. More slide here, on Veterans, what I like about this slide showing, a difference. Mostly. Just by age and veteran, status so you have veterans who are like. Myself as a veteran then you have veterans, who are enrolled, in, the. VA health, care system so, they're receiving some sort of care they're eligible for that care and, what. We see here is that the. Rate. Among veterans societies. In general is lower in the younger ages as. You get over age you. Know that 4550. Range it starts to increase, quite. A bit, and. It's also higher among those are actually the VHA or veteran, who's receiving those benefits of the VA health care center and. Again the hypothesis, for this might be well if they're, struggling. With health, issues whether. It's mental health or physical health issues they may, be a greater risk anyway, so that might be why it's. So high among BHA veterans. This. Next slide is showing. Some. Risk for suicide among persons who are in, inpatient. Psychiatric here, and after their inpatient, psychiatric care, so we know that there are very high risk in, fact. Since. 1997. Suicide, has consistently, ranked in the top five most common since in all events reported. In hospitals. Suicide. After psychiatric. Constellation, is extremely, high Sunday, to show it up to a hundred times higher I'm, a person's just discharged, for psychiatric care. Inpatient. Care than the, general population. It's, the same thing among US service members the, study I actually published with an unfortunate on surveillance Center we found that the rate was five times greater than, general. Active duty US military, population, over a decade of time. So. The rate is higher among those who are in some kind of inpatient, psychiatric treatment. Same. Thing in the veterans. Population. This. Study showed that 12. Weeks post hospitalization approximately. Five times the base rate of, the active treatment population. Fifty-four. Times that, original US population. So, if key about this information, is that we know that this is the high-risk group so, if working on interventions. We can really target this, group we can treat them while they're in care but also pay attention to their risk after they're discharged okay. So. Now let's talk about what causes a person to choose. To die by suicide. Unfortunately. I don't have enough time to go into all, of the, theories. About why, people die by suicide but. I can talk about the, primary risk factors, or protective, factors, these are really the, need to know, pieces, of information. There. Is not a single cause, to, suicide, and most often occurs, with, stressors, exceed, current coping abilities of stallin suffering, from a mental health condition.
Now. This is information or, a statement from the American Foundation for Suicide Prevention I, like, it because it's so simple, however. This is of course not account for everybody but, it is a very simple, explanation for what puts on that increased, risk. So. A risk factor is a variable, that increases. The likelihood of. Developing, a disease or disorder, examples, include any behavioral genetic, environmental or psychosocial, variables. So. In a moment here I'm going to go through specific risk factors for suicide. Protective. Factors are really through inverse of that these are variables that lower the likelihood of developing disease. Or disorder or in this case lowers, the risk for suicide, and, he's he'll, include behavioral, factors you. Know genetics, environmental, factors, really any other kind of psychosocial, variable, that can reduce the risk but. The impact of risk factors. So. Risk factors. Psychotic. Stories is a big one approximately. 90% of, suicide victims suffer. From mental disorder, time of death most. Common, are depression. Or bipolar disorder. Depression. Is, estimated, to be present, and at least 50%, of, all suicides. Lifetime. Risk of suicide among patients with country, depression, ranges from 2.8, about 50 percent, those. Suffering, from depression are, 25, times greater risk for suicide, than. The general population. So. For. Bipolar disorder this is probably the group with the greatest risk as, far as psychiatric disorders go 20, to 36 percent, of persons with, bipolar. Disorder attempt, suicide and, some. Studies are showing between 4 to 19% die by suicide that's. Way too high, the. Lifetime risk of suicide is estimated to be at least 15, times greater, than the general population. There's. Also current current conditions that they roll here including, Ziya disorder, alcohol. Substance abuse can also contribute, to suicide, risk. So. Alcohol is involved in more than 25%, of all suicides in, the United States. It's. 120, times more prevalent among. Adult. Alcohol abusers than in the general population, and. What. Reason why they play substance. And alcohol use in particular may play a role in, suicide. Is that. We. Know that about 1/3 people who died by suicide who. Die by suicide use, alcohol just prior to the death so. One theory about that is it's related to your call simony, often, suicide. Yeah, the act of suicide is not to consider to be closer, that's not always but in many ways it is and, that, alcohol may kind of play a role in that to sort of may. Contribute. To, impulsivity. And really, affect a person's cognition, at the time that they they're taking. Their lives or attempting. Alcohol. And substance use is linked to other factors, however for, example personal. Loss history, with these trauma access, to firearms even and so, it's really kind of a complex, miss. Factor. Social. And psychosocial. Factors, these. Are things such as socialized, social, isolation. Social. Exits, or loss, such as recent. Divorce or, separations. Patterns. Of aggressive, antisocial behavior. Is actually related to suicide. Risk. And. This is the biggest one almost of all and this is one of which I, think, we. Have. Some control over both, as individuals, and as healthcare providers and I think. Our. Leaders have, some control over this access. To lethal means and, primarily, I'm talking about here are firearms but it can also be drugs. Or, other means. Suicide. Means. Reduction is, an, effective, preventive, strategy. So some examples, may include storing. Firearms, and locked cabinets. Using. Trigger locks or. Storing the firearms with friends or family away. From the person. Another. One is locking up medications, or storing, those medications with a family member. And. Just, a little bit I'm going to get into some more about means, restrictions, or some, specific kind. Of skills and certain ways of doing it. Cultural. Factors is. Another important. Thing to consider stigma. Associated with asking, for help some people may be struggling with depression and, suicidal ideation, but, they don't go and ask for help because, they're concerned, about the stigma associated with doing so so, you. Probably have you. May have heard this has been a big issue with, the US military or veterans, you know willing, to go seek help the. US military, and the VA has done a great job at, expanding. Access and really dispelling. Stigma, and. Getting people to seek help by, working with really, all service. Members veterans and their family members but.
The Issue of stigma really is throughout, our society as, relates. To. Barriers. To access to get having access to services, this. Can be because of a lack of bilinguals service. Providers, we, certainly find this in some areas that, employ. Persons who do not speak English is a primary language. There. Can be sort of increased suicide, rates, or. Attempts. In, places that have, lacked, these service providers. Unreliable. Transportation. Can even be a factor, because it's impacts healthcare usage you can't get to where. Your. Counselor, is or some kind of crisis center that's a problem and, then of course the financial, some services to be able to afford. Cultural. Religious factors and, religious beliefs also, play a role. You. Know in some ways it can work in, both directions. Can. You have a preventive, effect but. Can also there, are some examples, where believe that suicide is a noble resolution to a personal dilemma and so that it becomes more socially, acceptable to, devices. These. Are important factors to consider if, you, come. Across a person or a person comes to you and they're in crisis, to be thinking about these factors. Some. Other contributing, factors history. Of trauma or loss such. As abuse as a child, bereavement. Family. History of suicide is. Also going to linked to increased risk. Economic. Loss this, is stress from. Employment. Or, divert, our divorce is also, linked to suicidal. Thoughts and, death. By suicide. Discharge. From inpatient psychiatric care, or a lack of continuity, of care and this is what I mentioned, previously this, is a serious. Risk factor. Also. Serious illness or chronic pain, and impairment, has, also been linked to suicide, and, as I mentioned earlier this could have something to do with why older, persons, may. Be a greater risk for suicide, especially if they're experiencing, chronic pain or any. Kind of other illness. So. Let's talk about some protective, factors. Skills. In, problem-solving. Conflict. Resolution, and handling problems in a non-violent way is a protective, factor. Strong. Connections, to family friends and community, support. This, is one that is I think, a relatively intuitive it's one that I'm very passionate about - variation in the interventions, that really focus, on this. Restricted. Access to highly lethal means of suicide pretty. Gain I'm going to kind. Of go over some more specifics, with that here at home it in. Cultural, religious beliefs that discourage suicide. Is for, self-preservation. Easy. Access to a variety of clinical interventions, is another protective, factor so if a person. Have access, to counseling. Or, even. Just knowing about a crisis, center having. Access to that is, a is, a protective, factor, effective. Clinical care for mental physical and substance use disorders. And. Support through ongoing, medical mental health care relationships. And so what I mean by that is that you know, to prevent suicide, and, self-directed violence, it's not just about you, know going in to see, a psychiatrist and you're done it's, an ongoing preventive. And treatment. Approach. That is. Effective, at reducing risk, for suicide, but. I'm not going through in this presentation. Are. All the types of treatments, that have been studied, and. Tested. That.
Specifically, Focused on suicide. Prevention there's a number of them they're showing that they're, highly effective. Typically. You. Know they're they're done by health care professionals, but. They are. Effective, in a number of randomized, controlled, trials are showing that they are effective, at preventing. Deaths by suicide. All. Right so let's talk a little bit more about these restriction. And reduction, so. What. Is means restriction. Reduction, so these are two B's designed to reduce access. Or. Accessibility. To means in the methods of deliberate self-harm in. Order to reduce the odds that their temperature will use a highly lethal means. Thus. Lowering the case fatality. Ratio, for suicides, and suicide attempts. That's a very academic definition. But that's just what it is, reducing. The odds that an attempt to really use highly lethal means is, really the more parsimonious, definition. Towards what I like so. Okay, so a person's, access to highly lethal means or methods, this is camera, use through there's some examples physically. Impeding, access this, could be through say for example easing, gun, trigger locks or. Even barriers. On bridges, like they've done major. Bridges from the Golden Gate Bridge for example has these barriers, that's, a physical, means. Restriction, also. Reducing, the lethality or toxicity, and they get a method. Example. Is like reducing carbon dioxide and, other vehicles which they've done. It. Can also be doing. Things with, medications. To reduce the lethality. And. We're also reducing, cognitive access. And, what this is reducing, a particular myth is appeal or cognitive, salience. In other words discouraging. Media coverage, of emerging, suicide, method so, a number of years ago there, was this. Situation. Where. The. Media was reporting a particular types of particular. Type of from. Means. Of suicide involving cooking. Charcoal, and I'm not gonna go into the details but. This started becoming popular in the media it's what they found is that this. Was primarily over in Asia what. They found is that people were watching, these four news reports, they were learning about this method and rates of suicide went, up sharply, by. That means because people have learned about it so, one way to reduce. Or. To Creek. Amis restriction, is what they call. Preventing. What they call media contagion, and that is preventing, the details of the information. Through. The media. So. I talked a little bit before about impulsivity, but among, persons who are newly who nearly died by suicide, attempt, twenty four percent so less than five minutes elapse between. Deciding, on, suicide, and making the attempt so what this is showing is that it. Is relatively impulsively, it's a pretty quick decision, even though people, may be thinking about it off and on having translate thoughts about it at, the time of the actual act of it it's, more immediate so. The, benefits, of a mean restriction. Is that, it gives time to the person to think to use coping, strategies, or, to completely prevent self-harm. So. Here's some more examples of means restriction and talked about a few of these already but.
One Of my favorites, are trigger. Locks these are basically little blocks of a key or they can be electronic, then, you actually go over the trigger of a firearm the. Department Veterans Affairs a number of years ago actually issued, these for free to veterans which. I thought was a wonderful public, health program. I would like to see that done here in Washington for everybody. Free trigger locks let's, have a public health campaign. To. Promote that I'm gonna get off my soapbox. Another, one is just having your gun steward, somewhere, else so if. You know someone who has a firearm when you know that they're in crisis or suicidal. The. Thing is to work with them to help them store the firearm sprouts and, I, do, talk I think later a little bit about more cultural, stuff with this cultural considerations in. That for, many people this relate my work with veterans is that they. Really. Appreciate. Their their right to bear arms if you're threatened to take away their firearm they don't like that and so you have to be sensitive, to the kind of the cultural implications of, doing that but, it can be effectively done when you just say look we're, could. You consider, having. Your buddy store, your firearm, or that family member, there, keep the ammunition separate, from it you'll still own your firearm you can really get it when I go on that hunting trip whatever but, what it does is it takes away that immediate. As I mentioned before that impulsive, access. To, that leaf or meat, blister. Packs what. These are you've all seen them they're basically a way of storing medication. So instead of having medication. Jar. Little plastic jar. They're, actually in like, a plastic, and aluminum thing we actually have to punch push through to get the pill out. Bubblegum. Comes this way now. This has actually been shown to, be an effective means restriction, for suicide, once they started implementing, these it's.
More The, reason why is that it, takes longer for the person to get all the pills out to swallow them all at once where if, you have a jar they can just pour the whole thing down all. At once and. There's been a number of studies worldwide. That I've shown that when they implemented these booster packs it actually reduced. The. Rates. Of suicides. Another. One I missed this before his medication, secured, or monitored by someone else so if a person. Living. With someone else that other person could sort of help kind of control that mad and. Maybe. Even help administer, it doesn't, work in all situations but. This. Can be an effective way, of means restriction and. Then removing. Ligatures. And. Devices, now, how. Do you do that in the home it's really up to a person but in healthcare, settings this is a major thing so hospitals. They. Have, to do this because. Otherwise. You're creating risk if you if you don't remove. Ways. That people can, hang. Their cells or suffocate themselves. It's. A little bit more about firearms I mentioned this already. Having. Guns locked. Away keeping. Them unloaded, and keeping. That ammunition lock, and stored separately, the, other big thing is education of farm safety I have, found this resource I really like it it's called lock it up die work it's. Through. King County Washington State, Park of Health there's. The web link to it definitely. Check this out it's a really great resource site, on this topic. There's. A consideration, just to kind of think about this a bit more, could. Blocking, access to, a low lethality method, such, as like locking up a medicine cabinet have. An unintended, harmful, effect leading. At timbres just substitute, for more lethal methods now. This is something that's really important to think about so I really, I personally, believe that when you're looking at each restriction, you really need to look at sort of everything that's in the person's environment I think. This could contribute to increased, risk if you take away one means they may go into another so you really have to think about everything. Okay. Now let's talk about signs. Of suicide, where's. All. Right so I'm going to go through some of the primary warning, signs and they're not in any particular order here these. Are things to be looking out for. Withdrawing. From friends family and society. Expressing. Feelings of failure and hopelessness. Rage. Anger, and seeking revenge. Acting. Reckless impulsive, or engaging in risky activities they're, one of the big ones there is, alcohol. Use. Speaking. About tidying, up affairs or giving away possessions. Threatening. To hurt or kill. Seeking. Access to pills weapons, or any other means. Talking. Reading or researching about death dying or suicide. Feeling. Trapped or, as if there's no way out of a situation. Increasing. Drug or alcohol abuse. Increased. Anxiety, and agitation. Dramatic. Changes in mood. Saying. That there's no reason for living no sense or purpose. In life giving up hope. Difficulty. Sleeping or sleeping all the time. You. Know if you're a supervisor, you may find that the person who's repealing late for work is can be a serious warning sign. Increase. For a decrease, in spirituality can. Also possibly. Be a warning sign now. Keep in mind that. These warning signs is not any combination. Of these just, these are all things that have been identified as, warning signs things to look out for. Now. If, a person. Goes. To a health care provider here, in the state of Washington, health care providers are now required. Basic. Kind of screening for suicidality, and, that. Screening, entails. Should. Entail. Really. A standardized, interview, and, some questions, about thoughts, of suicide and, there's several types of measures and assessment.
Tools That, aren't used however. Those are for health care providers for. Those of us who are not if we're if we're just everyday, people turn. About a co-worker family. Member or if we are a supervisor. Or manager. We. Have to be looking at these other kinds of behavioral, factors. And, then, what, I'm gonna show you next is also, key this, is how. To talk to a person who may be thinking of suicide, or be in crisis. So. Here's some best practices, you want. To ask questions. Interact. In a manner that communicates. Concern, and understanding is there showing empathy. Encourage. The person to talk but, do not pressure, them, and. You want to manage your own personal, discomfort, you know if you have you may feel anxiety or fear, maybe Terzi, frustration. You. Had your own personal or cultural religious, values that may, interfere with how you serve. Yourself, or dealing with them talking to a person who may be suicidal. And. You have to do this in order to directly address the issue. But. The most important. Frankly. Difficult question of all to ask is have you had thoughts of harm you're taking your whole life now. As you recall at the beginning I showed that one myth an assumption about asking, is does that actually increase risk, does. Not you. Really do have to ask about it directly, but. When you do ask about it directly. Do. Not ask the question so you're looking for a no answer you, want to be very open about it again. Empathetic, you, don't want to say something like you're thinking of killing yourself are you because. If you do that they're, not gonna want to talk to you that. You. Will want to explain. Confidentiality. Or DBT for duty. To inform as applicable no for the vast majority this, does not apply but, for, persons. Who are in, certain. Types of professions, such as health care professionals. In. Other types professionals. That have a duty to inform but required, to, notify. For. Example if a person may indicate, that they're going to harm somebody else we. Have to kind of do a certain notification, about that but. You have to consider, that how that may play a role and how your interaction with that person. Ask. If there is anyone who they'd like to call for support but definitely want to emphasize this one and I would do this from write that first time that you're talking to that person. Get. That other person available right away. Take. Immediate action to refer the person to him into a health resource, and. Stay. With the person if you can as. A health care provider. Myself. And as a manager, I always stay with that person they come to my office and they say I got having thoughts of preparing myself I just can't deal with things anymore I'm, not letting them leave my office I had want to make sure that were, they were they call it a warm handoff I'm either going to escort, them myself somewhere, which I've done before or. I'm going, to wait, for that family member to show up or I'm going to wait for our. From. Making referral to another health care provider I'm not going to let them go to the street and this.
Last One I put with an asterisk is document. I think it's important, to document what you do this is definitely the case for. Professionals. We, always have to take chart, notes you, as an individual, may, not be required to do this at all but it is something to consider definitely. If you are a health care professional or other professionals, such as a manager. So. Here's some more things to consider when you're talking with a person who may, be a crisis, you, want to remain calm. Lend. Your ears you know listen more than you think this gets back to that showing. Empathy and, today the pathetic. Listening. Let. Them talk. Maintain. Good eye contact, act. With confidence if, you can't and, this takes practice for, me to this. Use. Open body language. You. Don't argue in any way I want to emphasize that you. Want to be very, open. And listening, to what the person is telling you. Limit. Questions, to gathering information in, a casual, manner you don't want to make this too you know. Official. You know you want to sort of limit questions to just learning, what's going on in the person's life what's what sort of immediately going on. You. Supportive, and encouraging comments. Encouraging. What I mean is there, they're, you. Know they've. Used, the crisis line before they use the healthcare provider before they, talk to someone before about their issues that. They're having or if they have a safety plan. Related. To their suicide risk then. Encouraging. Use of that be. Is honest, and upfront as possible. So. Here's some best practices, really more specific, to the workplace, and for managers. So this. Is important, employees, need to know it's, okay to say to a colleague are you okay or you. Don't seem like yourself do. You want to talk it's. Important, to feel, that you can do this as an employee. In. A workplace but, as managers, we need to foster this kind of environment environment, where we're asking these questions that were able to talk to each other we're checking in with each other. Is incredibly, important. Encourage. Staff and, train managers to do this by creating work, environment. That encourages, communication sense. Of belonging respect, so the suicide prevention Resource, Center, is. A really great resource center. For information about this and I do have some links to that here at the end that I, do recommend that you take a look at. Identifying. Assist employees who may need help and. Know, what resources are available and, where, to refer now. This can what, I recommend is that if, you are an employer or a manager, that you find out where these resources are, in, your. In. Your work area if you're available contact. Your EAP professional.
They're. Gonna know what these are definitely. And. I'm going to show you a few resources here some national ones at, the end of the presentation. And. Be prepared to respond if there is a suicide, event and, what. I recommend here, is that I think that a lot of workplaces, they. Don't think about this it's always Oh after the fact now they're now the entire workplaces in crisis, and that's where he ap comes in they. Can dispatch out for, help but, this is something for us to be thinking about you know how do we think, about this ahead of time whatever, we do when we have an employee or, co-worker, who. Is in a crisis, one of the right things to do and then, what are our procedures, for if there isn't a bitch in, place. So. Let's talk a little bit about coping. With a suicide. Loss. So. Be prepared for powerful emotions. People. Who have experienced, a loss they, were all very shocked, confusion. They may have anger guilt, and depression. Everyone. Experiences grief in their own way in their own time really. Is no set time for, getting. Over it, be. Patient, this. Is for both the individual and for people who are, family. Members or. Managers. It. May be setbacks for that person, painful, reminders. Anniversaries. Different, things that can trigger memories, these. Are expected, stay. Connected to friends family. Supports. Support. Groups are extremely, helpful. Seeking. Professional help, is okay talk. To your health care provider the, CQ, consult. Intensity. Of grief does fade and things will get better it's important, to remember. That that, things will get better. Although. It can take a long time you'll be a very difficult road for things, to be better I. Do. Want to emphasize this. The. First bullet up here I have about people. Who turn into laws they came for depression, but there is also a link to increase suicidal, ideation, among persons who, have lost someone close to them too satisfied so. It's very important. To. Monitor. That and people who have lost someone close to them, and. I was just a conference. Recently with. The US military in there they were talking about how, when. There is a loss of suicide, how, many people are really affected, by that and there's some old data saying well it's you know it's maybe less than a dozen people but actually someone more recently there's study on it and, they find that you're on average, there's more than 120. People that are impacted, by one, death by suicide so. That's really the, people that are around that person like their family espouse. But. Also all the co-workers, think so many people are impacted, by a loss to suicide, and. That you really have to be thinking about what. Happens, if we do lose somebody, how it impacts everybody else. So. Here's a little more information really geared towards, for.
Managers You, know following your existing crisis response procedures hopefully, you have them so, I asked as a question or what are they do you have them. Provide. Input to employees promptly. Sensational. Details really, should be avoided but you should be able to respond to, questions but. Again avoid, those sensational, details. Because. When you provide those that, can actually increase the trauma for people if. I people can be trauma. Can. Experience, a significant, trauma just by, hearing. About the event so we have to be very aware. Of that. Providing, pleasure the median access support number one contact. Their EAP get them connected. Agency. Crisis response volunteers. Can be available as. Well as community mental health services. One, available resource this is a national. One as the American Foundation for Suicide Prevention survivor. Outreach program, and they. Actually have trained suicide, loss, volunteers, that can provide assistance also. I highly recommend you check out forefront, they're an, organization as part of University of Washington, in. Seattle they, also provide, some counseling services as well. And. Provide. Education, influenced. Suicide prevention in those complexities can help employees accept that, they were not in control of what happened so I'm talking about after the event is. To to military. Is the terminal brief brief people so we want to provide those briefings after, you that. Preferably. Its its management, that's there but also bringing in the AP professionals. And. Have them there to provide, those debriefings, to. Allow people to to, talk about it check, in with them see how they're doing, remember. This is something that a loss, like this it's. A major, impact a lot of people and the impact does not just go away after a week it, can persist for quite a long time. We. Must be aware of the spirit Accord we have to. Begin. Paying attention, to how, it's affected, in their network, place over time we. Need to encourage managers, to check in on employees, to see how they are doing in coping, so this should be something that they, need to be doing really individually, talking. To their employees. See. How they're doing and. Managers. Themselves need, to be checked in, so. Their managers, I, think, EAP. Is all they should be checking because. They can have serious, feelings of guilt and grief, themselves. Knowing that well maybe they didn't do something when they can where they could ever should have they may have those feelings it's, so so important to check in with them. This. Is also there's some recommendations. Really for employers, and for managers given employee option to attend if you're all memorial. Service they'll, be aware that criminal memorials such, as pictures, employee. These. Can actually can trigger traumas, in the workplace so. Just. The appropriateness, of these, and. Give employees options and support your sister and loyal service as they can as this can help with healing and so if there is a workplace. Kind, of Memorial or something that's going on that, can.
Actually In solve be eternally healing, experience. So. In the next slide here I'm going to show you some resources these, are, primarily. National resources, but. These are excellent. Resources I highly recommend that you take a look at for more information, many of these resources have. Pamphlets. And, kind of educational, stuff that you can download. And. You can certainly give to fellow. Co-workers, and you should definitely read or solve National. Suicide Prevention lifeline. They. Also have direct links to crisis, line so. I highly recommend that as a resource, suicide. Prevention Resource, Center that site, has. Some really great stuff for workplace. Suicides. I highly, recommend it I mentioned. Forefront, that's the University of Washington, outfit, really. Awesome group up there and. They've got some really great materials. The. American Foundation for Suicide Prevention is, another one and. The. World Health Organization, actually has some good resources available, they have a resource at work could. Have a manual I guess you'd call it it has a bunch of recommendations. For. Suicides. In the workplace. So. In closing let's. Learn about the problem, of suicide. Unless. Dispel, the stigma associated. With, suicide, and in genomics so let's talk about encourage. Others just talk about it this really has to be the first step and let's. Look out for each other and strangers, too this isn't just about what. Health care providers need to be doing to people with mental health conditions this. Is for all of us we all need to be aware of the problem with suicide and. We need to be looking out for each other it's okay to ask others about how you're doing and if. You are smart and you've got you know if you're smart by having those resources noble T know where to get them you know where our crisis line is. To. Refer and say look here's a resource to you or, hey maybe you should go talk to somebody and be that kind of courage a friend to that person that, can save a life. So. I do thank you for participating in, this, webinar I do have you can see my emails there you're very, welcome to shoot. Me an email with any questions, I, do believe that this has been recorded so this will be available as a resource to you. And I can also make the presentation. Available I often just put. It up on my personal website for, free of course you're. Welcome to download it if you wish or just shoot an email I'd be happy to send it to you and, I. Have, I guess we have a couple minutes here we can take some questions if, there are any. So. One question is from Cheryl Flynn she'd like to that Cheryl would like to know if there's these, statistics. About, persons, with terminal, diagnosis, for chronic pain disorder, lates. Yeah so this question has to do with is. There any statistics about persons with terminal, diagnosis, or chronic pains or regards. To suicide risk there, are top my head I can't tell you what their that rate is it's actually probably a smaller, group but that group is really high risk we, know this already as.
I Mentioned earlier in the presentation we, think that that's why it may be higher suicide might be higher among. Persons. Who, are a, little, bit older but who do have some chronic health conditions, pain, is a big one. This. Question is what's the likelihood that the media will reduce its fascination, with human death, I. Remember. The the Don Henley song dirty laundry I do remember that song to race off they. Seemed desperate to sell newspapers well, this gets back to what I was talking about earlier about the media contagion effect and, I have a personal. Concern right now about, these. School shootings and, how the media, reports these, and how it may actually be increasing the mysteries I don't know if anyone else is talking about that but I'm talking about it because, we know this about from, the suicide literature that just, reporting, these things that's saying how they did it going through all those details actually, increases, risk but. In. 2012. I published a paper some colleagues called social media suicide, prevention public, health concern and in, that paper we talked about the pros and cons of the media reporting, suicides, not really, what we have is an issue also free speech so we want to be able to have the, press be, able to report things because I think the public Snowbell what's going on in their communities however. The. CDC actually published, some guidelines, about media, reporting, some years back and. So hopefully the media outlets are following those guidelines and. Really limiting, the details about what they're reporting. Have. Another question here is. The does the Veterans, Affairs approach. To, asking, the question, have had you thought thoughts of harming your taking your own life, simular. Or different, than how many we've generally asked the question. Okay. So the question is, how.
Does The Department Veterans Affairs ask that question about having to thinking about suicide, or yourself. Versus. Her recommendation to the general public or sort of I guess really just serve the clinical literature. The. VA like it like any kind of health care system they may have their standardized, approach. For. Asking those questions and, how they do it. What, I'm recommending here, is just straight, up a task because, that really, is what the media or what the literature shows you ask the question, you. Know. I think Kiki. Like what I was trying to emphasize and, sort of best practices, and doing those you you really wanna have that relationship. Going where the person feels confident. And okay. Talking, to you you, don't want to be in a position where you're asking questions is if you're interviewing them like they're going to get in trouble we. Do not want that and, clearly we have a concern if a person is employed and, they're going and telling your manager something about this. There's. That concern of stigma well my mayor is going to fire me or they gonna take me off the job I'm, gonna lose a raise, those. Kinds of things but that's why we have weight assistance, programs. Right that's why ploys, and individuals, out there should. Be encouraged to talk to your EAP if. You're having these concerns. Okay. I've got at least one more question here have. The rates of people affected by depressions, I had gone up with the US suicide, rate excellent question this, is someone, is thinking about about. Public, health and statistics, here, you. Know I think the top my head I don't know what the rates are on turn anxiety disorders and depression but they are quite high I think, they have gone up in some groups, how. That currently, specifically, with the suicide rate has not been a strong correlation as, far as an increase great I'm, more familiar with the data from the US military and the Yanks I've worked in that field for many, years and. We tried, desperately to figure out what is causing an increased trend, among. Veterans. And active-duty. Service members and. These. Things themselves the mental health conditions, are not. Increased. Nose is not really necessarily direct correlate, with. An increase, in suicides. However we do know that they are correlated. As I mentioned earlier that depression. Certainly. Is associated, with suicide. It's, been also discussions, about things like post-traumatic. Stress disorder and, deployment. To combat zones among veterans does that increase risk, well those themselves. Have, not necessarily been, linked. To increase. Or. The increase, in risk among, veterans, or active service, members there was a seminal paper published, just a couple years ago that showed that it was not related now, this does not mean that persons.
With Post-traumatic stress disorder or. Suffered. Some serious traumas, are not, at increased risk for depression, and potentially, suicidal thoughts, or risk. For. Death by suicide but, in itself, is not really the predictor. Okay. Alright, again you have my contact information. I feel free to contact me thank. You Matt for for hosting this today and, thank. You so much for attending this webinar that, you found useful.
2018-07-03