Cell And Gene Therapies Day 2
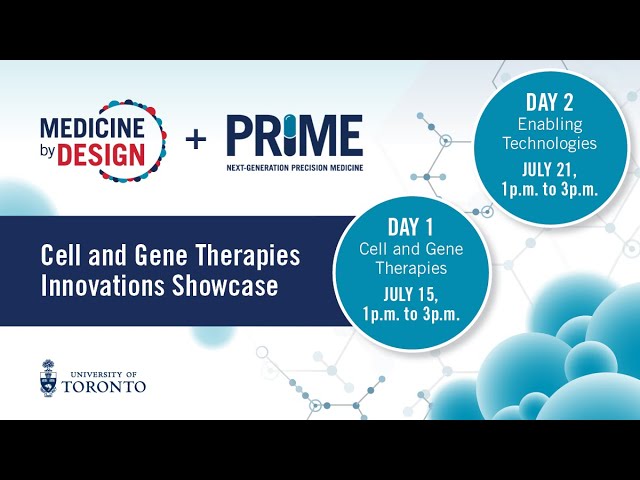
afternoon everyone thank you so much for joining us for the cell and gene therapy's innovation showcase i'm shayna kelly i'm a faculty member at the university of toronto and also the director of prime i'll be moderating our session today we uh this is a two-day event uh first day was was last week now we're moving on to kind of the the enabling technology side of cell and gene therapies we have a really exciting lineup for you today but first let's just talk about a few housekeeping notes uh we are going to record today's session so that folks that can't join us right now can can view the presentations later live captioning is enabled you can see the captions if you click the live transcript button at the bottom right of your screen uh the chat because we have a fairly large group joining us today it's been disabled use the q a box to leave your questions we're going to have all the presentations kind of back to back and then we'll have panel discussions just to go through the the questions that you bring forward we would love to hear from you uh so please do type out your questions in the the q a box and so then uh before we get going uh we should also uh just do our our land acknowledgement despite the fact that we're doing this virtually we wish to acknowledge the land on which the university of toronto operates for thousands of years it's been the traditional land of the huron wendot the seneca and most recently the mississaugas of the credit river today toronto is still home to many indigenous people from across turtle island and we are very grateful to have the opportunity to work on this land so before we get going today uh i just wanted to say a few words about prime so this event is being co-sponsored and was co-organized by medicine by design and prime you heard about uh medicine by design in the last session uh it's a wonderful program that we have based here in toronto focused on regenerative medicine very uh core application of cell and gene therapy but today i'll just say a few words about prime before we get going prime is an initiative based at the university of toronto it is focused on next generation precision medicine uh the development development of new therapeutics diagnostics new ways of looking at disease biology across many different indications it brings together over 80 faculty members from four different faculties at u of t from 15 different departments we also have 150 trainees and our mission at prime is to really elevate research increase the research funding that our campus sees in these areas really empowering collaborations training a new generation of multi-disciplinary and translational leaders creating community we have a large ecosystem in toronto we really want our community to be as connected as possible and we also are quite focused on building toronto's biotech ecosystem so that's that's prime in a nutshell uh this is a very translational and entrepreneurial group of people lots of companies started venture capital raised uh all with an eye towards impact in the the biomedical sciences um i won't spend too much more time because we're kind of ready now i think to to move on to our next speaker but hopefully that gives you a sense of of what we do at prime at the university of toronto so then without further ado i think i will uh introduce our first speaker christine yeah if you want to go to the agenda so we're running this from one to three today as i mentioned we're going to have back-to-back presentations we'll have some discussion and then we'll move on to a second set of presenters and then have some discussion with them and then wrap up right on time at three o'clock so for our presenters i'm going to turn my camera off but if you're going over time i'm going to turn it back on so that you are aware that your time is up and uh we just need to keep things on time to the extent possible so without any further ado i will introduce our first speaker today uh who is maude uh dumont lagasse and uh she is a uh or is the associate director of r d and special products at excel thera which is a montreal-based company developing bio-engineered solutions for blood cancers mod completed a phd in molecular biology with a specialization in immunobiology uh at uwm before joining excel thera in 2018. today she's going to present work done in close collaboration with the hematology team leading clinical trials uh at a hospital montreal and this work explores how cord blood expansion increases donor availability for different populations so please take it away bond thank you so much for the this introduction so i would first like to thank the organizers for giving me the opportunity to talk about the work we do at excel thera it is a highly collaborative work as mentioned by um uh by shanna um so i'm just going to share my screen right away and then uh screen 2 and then present let me let me know if you see my presentation i think it should be fine we don't um your screen sharing but that you need to double click to enter full screen mode editing controls all right just bear with us for a moment everybody okay can you see it now now uh yes if you go into full screen mode we should be good to go is that okay perfect okay thank you all right okay so uh exothera is a cell therapy company based in montreal that was created after the discovery of the um-171 molecule by the laboratory of dr slavajo and dr marinie at inverse de maria so the molecule was developed and optimized between 2010 and 2013 for its property to expand uh stem cells hematopoietic stem cells uh ex vivo um following the the good results that they had they decided to create excelfera in 2014 and continue with pre-clinical development and the first clinical trial using the um-171 cord blood transplant was initiated in 2016 including mostly patients with hematological malignancies who liked a donor so if you're interested in the full trial results they were recently published by dr cohen in the landsat hematology in 2020 so before we we go to the results of the trial we might ask the question why should what is the use of expanding cord blood stem cells so emitopedic stem cell transplantation can be performed for from three different stem cell sources uh the most commonly used are bone marrow and mobilized peripheral blood so these these two sources of stem cells are collected from adult donors that are specifically matched with the patients um they represent the standard of care for hsct however due to the maturity of the cells contained within either bone marrow or peripheral blood um the the donor requires to be very stringently hla matched to the patient um this makes matching more difficult between donor and recipient and uh leads to several months of delays between diagnostic and transplants for a lot of patients but also to a significant proportion of patients having access to no donor basically so that's where cord blood becomes interesting cord blood can be collected at birth so from the umbilical cord blood without any risk to the babies and the mothers and due to the immaturity of the cells that they contain they require less stringent hla matching which makes it easier to find a match between uh donor and recipient so historically the minimal hiv matching that was recommended was four out of six actually genes or actually alias and uh with uh more precise um allele uh sequencing uh now uh we we translate that into five out of eight actually matched requirements so cordless cordless units are cryopreserved in cordless banks worldwide and are readily available for transplantation which is a huge advantage as patients waiting for a transplant can see their disease worsen if they wait too long if they have to wait too long basically the bad side of cord blood is that most cord blood units contain a low number of cells translating into a low stem cell dose for adult patients especially and this has been associated with several transplant related complications these complications can be summarized as delayed engraftment and immune reconstitution leading to an increased risk of graft failure and increased infection incidence and severity these both combine to increase the risk of transplant-related mortality making this graft a little bit more unsafe than what we would see with bone marrow or peripheral blood and so that's why expanding blood stem cells appears on it as an attractive strategy to prevent the low cell cell dose issue of cortland so that's where excel terra's technology comes in the manufacturing process is quite simple we basically select a single cordless unit that is specifically matched to a patient that was recruited within a trial and once we receive the unit we can thaw it and perform a cd34 positive cell selection so the the separation of cd34 positive cells from uh the rest of the cells contained within the grass is done through immunomagnetic bead enrichment using the clinimax system that is approved for clinical use um the cd34 positive cells are enriched in metabolic stem and progenitor cells they will be placed in culture in the presence of um-171 for a period of seven days with other growth factors and after this seven-day culture period the cells will be washed to remove the culture reagents and the um-171 molecule and only the cells will be formulated and cryopreserved for future use the cd34 negative fraction uh which contains more mature cells so including the t cells are also uh prepared formulated and cryopreserved but there is no culture involved with these cells and both products are infused together to the patients and are important to to provide prompt um hematopoietic reconstitution and early post-transplant immune protection within our trials we have seen very uh very encouraging results with a prompting graftman we saw the 100 neutrophil per microliter threshold i think quite early so at 9.5 days which is earlier than what is seen with other stem cell sources and patients also benefited from a very quick resolution of fever so um compared to to cord blood or bone marrow expansion there was a significantly lower uh time to fever resolution uh the graphs are well tolerated leading to a fast immunosuppression withdrawal with most of the patients being off immunosuppression withdrawal at one year which is not the case with a standard standard of care basically all of these combined to a very good what we call grfs so drfs is gvhd and relapse free survival it is a metric that encompasses all the important outcomes following a transplant so patients um patients who succeed with this metric actually do not have a grade three to four or qgvhd moderate to severe chronic gvhd uh they don't relapse and they survive basically the transplant and compared to a cohort of 907 patients transplanted at university of minnesota which is shown in gray here um we the the patients uh receive transplanted with um 171 expanded cord blood showed very good grfs um the hum-171 graphs uh show a very different cell composition so uh in a study where we we that i led where we uh we analyzed the immune reconstitution in patients in our patients transplanted with un-171 grafts we compared um our patients to a cohort transplanted with unmanipulated cord blood so which you see in red here in our patients in blue and while the num the total num the number of total nucleated cells was quite similar between the two groups there was no significant difference the cell composition differed greatly so we had a 17-fold higher dose of cd34 positive cells which contains the stem cells um thanks to the um-171 expansion but we also had a lower dose of cd3 positive cells and this is due to the manufacturing steps uh necessary for the separation of cd34 positive cells for the culture so we wondered if that might translate into different and different clinical results basically interestingly the t-cell reconstitution was quite similar between the two cohort so here i show uh cd8 and cd4 t-cell counts at 3 6 and 12 months in both cohort and basically what our results show is that we didn't see any differences in the numbers and the phenotypes of the t cells so the lower t cell those infused with the um 171 graphs does not seem to result in any delayed t cell reconstitution we decided to go a little bit further into the analysis of t cells by performing tcr dtcr sequencing and um the results were quite interesting basically the um-171 patients presented a higher t-cell diversity at 12 months so this can be shown by the number of unique t-cell clones that can be detected within a sample but also with metrics of diversity such as the uni index which is planted in the paper that we published in stem cells translational medicine um interestingly the the increase in t cell diversity was most pronounced in younger patients so patients under 40 years old which was also accompanied by an increase in naive t cells and recent thymic immigrants suggesting that the expansion might actually lead to an enhanced thymopoiesis in younger patients this correlated with an increased common lymphoid progenitor frequency and potency within our graphs so these are in vitro uh assays but basically what we've observed is that the concentration of common and freight progenitors is increased with even 171 cultures but also for each uh clp or common progenitor cell plated the number of cells contained within a colony forming unit was higher meaning that they were more active so that might be one explanation to um to the enhanced timeline policies that we observed and um how this translated for the patient is actually better immunity so we comp we compiled the number of infections and the severity of each infectious events uh that occurred within our two cohorts and basically what we saw is that the um 171 patients shown in blue here benefited from an early protection against uh great well bacterial infections both grade two to three and um grade one two three and um this this was particularly uh clear in the early post-transplant period the first month after transplantation where the patient is most at risk actually we also saw that the viral infections were lower for the grade two to three viral infections were lower for patients transplanted with um-171 cord blood so um this means that not only in terms of t cell numbers we have a similar reconstitution but in terms of t-cell diversity and t-cell function we seem to have an advantage linked to the um-171 graphs finally one of the very important aspect of the um-171 expansion is that it increases the pool of suitable cord blood units that are available for patients so here i show uh three graphs basically it's the same data set but that adapted for different patient weight so the minimal cd34 and tnc cell dose required for single um unmanipulated cord blood or double un unmanipulated cord blood transplantation makes it um uh harder to find a donor for patients as um only as a pro a very small proportion of the of the cord blood banks are actually available for these patients by allowing the use of smaller cord bloods um 171 expanded grafts actually increases the the proportion of cardboard units that are that contain sufficient cells for patients meaning that for instance for a 100 kilo patient um if a physician would like to perform a single unmanipulated cord blood transplant you would have to choose within point five percent of code blood units stored within a cordless bank while with the um 171 it could the the physician would have access to 23 percent of corporate units which makes a big difference basically and this higher um donor availability also translated into better hla matching within our trials and so for our first uh phase one two trial we've seen that approximately 50 percent of patients had access to a better hla match cord blood than what would have been possible without expansion and um approx more than 75 percent of them had a six or seven out of eight hia match units which is very good um we'll need you just to okay you were yeah yeah i'm done thank you and so basically in conclusion our results uh suggest that the um-171 expanded cordless graphs are safe and effective leading to low transplant related complications and providing good immune tolerance the immune reconstitution is prompt and robust we showed high that we had high t-cell diversity at six and twelve months post-transplant with a better immune protection against uh bacterial and viral infections and basically uh by allowing uh more access to more cortland donors the patients also benefited from better hiv matched units so i briefly want to thank all the the people that have been involved within these studies and i will be happy to take questions at the q a sessions at the end of this uh this group presentation thank you okay thank you so much mod we will come back to you in in a bit with some some questions uh for now we're going to move on to our next speaker ronnie chidiak who's a postdoctoral fellow in the lab of stefano jay in the leslie dan faculty pharmacy at the university of toronto ronnie has a phd in pathology in cell biology from university of montreal his current research is focused on modulating the wind pathway using novel antibody based agonists that selectively target frizzled receptors as a path towards regenerative medicine therapy uh ronnie was one of our 2019 prime fellows and recently got a really nice new fellowship from the bright focus foundation all right ronnie thank you shanna can you see my slides can you hear me yeah looks good perfect thank you so much and i would like also to thanks the organizer uh for the invitation so it's a great pleasure for me actually today to talk to you about our recent work in the lab introducing the friso iv lrp5 antibody as a drug candidate for the treatment of the vascular retinal body so when beta-catenin signaling actually is required for the formation and the maintenance of the blood retinal barrier which is characterized by the formation of a tie junction between endothelial cells among the ten different physical receptor fissure four is and express endothelial cells and act as a receptor for the secreted protein norin noren bind to frizzle 4 along with lrp5 as a core receptor and needs also the expression of the t-span 12 at the third receptor in order to activate the wind beta cathedine signaling which leads to the expression of some of the junctional proteins such as the chlorine files a decrease and the down regulation of the wind signaling can lead to a decrease in the expression of the junction of protein which leads to an increase in the vascular leakage and this is a hallmark of multiple retinopathy diseases such as a diabetic retinopathy and retinopathy of prematurity which could lead eventually to blindness so genetic loss of function studies have shown that down regulation and knocking out ndp lrp5 or frizzle 4 or t-span 12 or even beta-cadent can lead to a decrease in the barrier formation and the border function in the retinal however interestingly when they when this study expressed a stabilized version of the beta-carotene and endothelial cells this lead to reverse the phenotypes that was seen in the frizzle iv and the noren knockout where the the barrier function is promoted and then there was a reverse and the phenotype so there was enhancing and the very barrier integrity in the retina so this led us to think that the pharmacological activation of the frizzle four but the catenan signaling and endothelial cells could represent a novel strategy to promote or restore the barrier function and we think we have the right tool for that so uh recently uh like we have a long collaboration with dr sidhu is at the uft an expert in protein engineering where we recently we published an e-life in 2019 a paper where we introduce a tetra violent antibody as a novel tool to selectively and at will activate one or multiple physiodeceptors so these receptors act as a wind uh similar to the width purified protein so they activate very selectively the wind but the catenan signaling and knowing that wind signaling is downregulated in multiple diseases we thought that this could be a valuable tool in order to selectively at the receptor level activate the wind signaling and could be very valuable for the regenerative medicine and today i will be showing one of the first application of this tool using the frizzle 4 and rp5 antibody since we know that frizzle 4 and rp5 as i introduced are important for the barrier integrity so the physical four every five what we call this f4 and five point thirteen which i will be referring in my presentation as the friso four agonist is also a tetravalent antibody so it has a two diaboli on each side of the fc on this side you can see that it's a very selective to bind to only frison four among all the different physical receptors and the other side it binds to lrp5 but not rp6 so we have a molecule that can bind selectively to these two receptors fissile 4 and rp5 so we asked the first question we asked is whether the frizzle 4 agonist can activate the went by the cathedine and signaling endothelial cells so for that we treat it in the t cells with either noren or frizzle 4 agonist and we monitor the accent 2 rna expression by qpcr and as you can see here both noran and friso 4 agonists can activate the wind signaling with wind but academic signaling however our physical 4 agonist has higher potency than the northern so the next question we know that noren depends on the t-span 12 in order to activate the wind signaling so we ask whether the frizzle 4 is also dependent on the t-span 12 well as you can see as expected if we down regulate t span 12 using nsrna this abolish completed this signaling and induced by the norin however this was not affected by the treatment of the frizzle 4 agonist so we concluded that the frizzle 4 and lrp5 clustering that are that is triggered by the friso 4 agonist is sufficient to activate the bacterium signaling and endothelial cells which is mimicking northern ligand so uh one of the first uh feature earliest feature of retinopathy is a vgf mediated breakdown of the blood blood retina barrier and vgf increased permeability in the t results and that's why the standard care fuse uh the vgf therapy the anti-vgf as a therapy for multiple retinopathies so what we ask is whether our fizzle 4 agonist can decrease or block the vgf increased permeability and in the diesels so for that we treated our entire cells with vgf and as you can see this led to a decrease in the localization localization and the expression of junctional proteins such as one here clothing three and clothing five and consequently this led to a significant increase in the permeability across the monolayer of endothelial cells however interestingly when this was when pgf was co-treated with frizzle four agonists this completely blocked the permeability and rescued the phenotype seen with vgf and this in part uh due to the restoration of the junctional ex protein expression such as so one potency and chlorine five as you can see so we concluded that the frisol four uh rp5 agonist treatment can promote the entire cell function in v2 so what about in vivo so we used two different models in order to test our fizzle 4 agonists in vivo the first model we used a t-span 12 knockout mice so these mice display a defect in the blood retina barrier and they have a malformation in the vascular flexes and so what we've done is we injected the mice with either an isotope control or a frizzle for a agonist from starting from a p5 to p20 and then we stand for the retina with either isolectin to stain foreign cells or igg to probe for uh barrier defects and as you can see in the t-spans as expected and the t-span 12 knockout mice you can see that there was a massive uh extravasation of the igg as indicating that the vessels are leaky and also this there was a huge malformation in the vascular plexus the deep layer was completely gone however when we treat the mice with the frizzle for agonist this completely rescued the phenotype as you can see that with a mice that are injected with the freezer for there is no leakage of the igg and the vexilar plexus is is not affected so uh we even checked for the barrier function by the expression checking by investigating the expression of the cloning five and as a tie junction and the pl vap as in the tsl fenestration as you can see and as expected uh and the p2 p t span 12 with the isotope control you can see that there was a down regulation of the chlorine 5 and an increase in the pr vap expression indicating that there is a barrier defect however this was restored and completely rescued when we uh inject the mice with the frizzle for agonist so protein five is back again on the uh at the junction level indicating that uh where that there is a there is a promotion of the barrier function so we also use another model so we tested our physical for agonist if it can reduce the pathological neovascularization and the oxygen-induced retinopathy model which is a model of diabetic retinopathy and relative retinal body of much premature maturity so what we did is that we kept the mice up to p7 in a regular room air and then at p7 we move the mice to a 75 percent oxygen chamber where this could lead to a vessel loss and then at p12 we we inject the mice with either a vehicle anti-vgf or a physical four agonist then we move them back to a regular room er where this will induce a neo-vascularization step and then we sacrifice the mice at p17 and as you can see our fizzle 4 agonist can significantly decrease in neovascular reduce of pathological neovascularization at this similar to what we got with anti-vgf which is which indicate that our physical four agonists could be a tool to treat our diabetic retinopathy for example so the flag is a very powerful tool and very valuable tool as i mentioned when signaling is downregulated or modulated in different diseases so we can now treat selectively different friso receptor in order to modulate the activation of wind signaling and try to treat uh these diseases but what i've showed today at the at the level of the of the frizzle 4 and the retina we can use this as a promising tool in order to treat the retinopathy diseases but the similarity between the blood retina barrier and the blood brain barrier led us to think that the frizzle fork can also work and to treat the leaky vessels in the brain which can cause also other diseases such as like central nervous system disorders such as stroke glioblastoma and others so for that i would like to thank all the people that collaborated to this work especially all the members of the angels lab the member of the sithus expert and the protein engineering junkies lab which are expert and uh vascular retinopathy models and clerical therapeutic which provided uh valuable resources uh founded by stefan and dev at the uft and also the funding agency and for you for listening thank you so much all right thank you so much beautiful work so we'll come back with some questions uh in a bit our next speaker is penny gilbert penny is an associate professor at u of t in the institute of biomedical engineering and she's a faculty member affiliated with prime she received her phd from the university of pennsylvania did a postdoc at stanford before joining u of t in 2013. she's the recipient of an ontario early researcher award and holds a canada research chair and endogenous repair and today she is going to talk about preclinical models of human skeletal muscle function so penny will turn it over to you it looks like maybe you are uh like in there you go perfect take it away okay perfect so um thank you so much shanna um as shanna noted the focus of research in my lab is on skeletal muscle tissue and skeletal muscle is the most abundant tissue in our body and it's comprised of bundles of multi-nucleated cylindrical muscle cells that contract in response to human intent to enable functions like walking and smiling and swallowing but there are situations where skeletal muscle integrity is lost resulting in diminished quality of life and in some cases even death one of these examples is duchenne muscular dystrophy which is caused by mutations in the dystrophin gene and dystrophin is really a giant protein and it bridges the specialized cytoskeleton that's on the inside of muscle cells to the proteins that are embedded in the plasma membrane of those muscle cells that then engage with the extracellular matrix outside to support contraction and so without this protein bridge dmd patient muscles decline in health with time and this results in cardiorespiratory failure in the third decade of life and at the moment corticosteroid treatment extends life by delaying disease progression but this really does not prevent death and so both gene and cell therapies are being tested as strategies to improve or extend life or even serve as a cure and at the moment mice and dogs with mutations in the dystrophin gene are commonly used to test promising dmd therapies but what i'd like to talk about today is the possibility of humanized preclinical muscle assays kind of bridge the gap between these animal studies and human clinical trials so 2d cultures of multinucleated human muscle cells offer a really easy strategy to test batches of cells for myogenic tendencies or the ability to target dystrophin by gene editing strategies and while 2d cultures offer a lot of benefits studies of function are limited in this context owing to the detachment of the cells from the culture dish upon contraction and so this is really where 3d cultures start to take center stage they're really well suited to maintaining human muscle cultures for several weeks lending to enhanced contractile maturity and allowing for studies of cellular function like strength and calcium handling in the case of dmd it's contractile movement so walking and running that potentiates muscle cell membrane damage and leads to those uh unending cycles of degeneration and regeneration that are hallmarks of dmd so the ability to study these features of dmd in muscle cultures is really contingent on these uh the ability to stimulate contractions and that was what motivated our interests in going down the path of trying to model dmd in culture now the basic recipe for creating 3d muscle tissues in a dish is pretty straightforward you need a source of transit amplifying myogenic progenitors you're going to need a protein-rich extracellular matrix to suspend the cells within and act as a hydrogel and you need some sort of culture device with a couple of attachment points usually that support the establishment of uniaxial tension so those myogenic progenitors can be immortalized or primary cell lines that are derived from a patient or human muscle biopsy they can be pluripotent stem cell derived or myod converted fibroblasts or from other sources and then here i'm showing you one example of a very very simple device where those attachment points that i referred to are literally just two pieces of velcro at either end of a channel that is then filled with the cell extracellular matrix slurry and what we find is that over a period of a day those cells that were evenly spread in the well will self-organize to create a nascent tissue in the center between the two attachment points and within a week the tissue is populated with aligned and multi-nucleated and striated muscle cells as you can see here and they are contractile at this time point so we have invented my team um alone and also with collaborators have invented a number of different types of platforms with which to manufacture and study 3d muscle tissue function in culture and so this first one that i'm showing you here is a 96 well flexible rubber device where it's possible to cast arrays of tiny little muscle micro tissues um that are across two attachment points that are flexible rubber posts and the deflection of those posts can be used to quantify changes in tissue strength over time this second example um is an eight well device that's made of a hard plastic in this case um and can in theory be scaled to a 96 well format and in this case the advantage of the system is that it's an inverted design and so in this case the tissues are cast in close proximity to a glass coverslip and hopefully what you can appreciate here is that the tissues are spanning across these two long rigid um but but long posts and because they're long the tissues when they contract will deflect those posts and it's possible to get measurements of strength in the context of this device but at the same time because the tissues are close to the glass coverslip it's also possible to do high-resolution microscopy which is a really nice feature of this system and then more recently we've been working with allison mcguigan's lab and we've adopted a very very simple paper scaffold that supports both 96 well and 384 well footprint arrays of 3d muscle cultures for analysis and so all of these platforms offer an opportunity i think to provide a quality control assay for therapeutic muscle cell batches or to evaluate gene therapies using a humanized assay of muscle function and each of these systems have their advantages and also their limitations so it's a context dependent so what types of metrics are possible in this system so i'll just um highlight some of our recent work we produced muscle micro tissues using cells from dmd patients and we established protocols to be able to assess the contractile apparatus using immunohistochemistry and electron microscopy and we studied tissue strength and calcium handling downstream of stimulated contractions and perhaps most importantly in the context of dmd biology we adapted assays of muscle membrane integrity that are typically employed in humans or in animal models of dmd to instead be implemented in our 3d cultures and these included the creatine kinase activity assay the evans blue dye assay and we have also employed electrophysiology to explore membrane integrity in these 3d cultures and what i'll just point out is that very importantly significant tissue level distinctions between healthy and dystrophic tissues only arose in our hands after induced contractile activity which makes sense because this is also what we see in patients so let me show you two very short examples and then we can discuss more in the discussion period so with our colleagues at utm um my team prepared healthy and dystrophic 3d tissues and then our colleagues conducted electrophysiological analyses of the single muscle cells that were in each of the tissues and so here's an example of the data that's obtained using sharp electrode intracellular recording and so in this case we're looking at the resting membrane potential each of these dots is an individual muscle cell inside a 3d tissue and the resting membrane potential is something that's determined by primarily two factors the differences in ion concentration of the intracellular and extracellular fluids and the relative permeability of the plasma membrane two different ion species now in our body a healthy muscle cell has a resting membrane potential of about minus 70 to minus 90. and so it's notable here when we look at these muscle cells that are made from healthy muscle donors that we can find a resting membrane potential that is matching what we would expect in a human and this is further notable because studies in 2d cultures that have tried to measure the resting membrane potential of human um myotubes have not been able to achieve these sorts of resting membrane potentials that get so close to what we see in the human body and then these two cell lines here are tissues that are made with dmd cells two different patient lines and hopefully what you can appreciate is the dmd myotube sarcolemma is significantly more depolarized and that's suggesting that the membrane is leaky and this is consistent with what we would expect from a dmd muscle tissue where you're missing dystrophin protein and that that link to the ecm is disrupted so as you'd hope we can test the influence of therapies to modify the integrity of the strophic muscle cell membrane so here is one of a few examples that we have where we treat the muscle cells in this case with a beta one integrand activating antibody and that serves to enhance the ability of the cells to grab onto the extracellular matrix around them in the absence of dystrophin that would help would normally help to potentiate the forces through the cell membrane and what we can see following this treatment when we look at the resting membrane potential is here's the parental cell line and the muscle cells that are being tested and you can see that upon treatment with either of these treatments igg4 or the beta 1 integrand activating antibody that we see that the resting membrane potential becomes more negative it's moving closer to this healthy control and that tells us that the integrity of the membrane has improved downstream of these two treatments i'll just note that the igg4 treatment is one that is being tested in clinical trials in people so next is an example of a phenotypic analysis where the outcome is contingent on stimulated contraction so here we're looking at electron microscopy images of 3d muscle tissues from healthy cells here on the left and from dmd cells here on the right these are two uh different patient lines and hopefully what you can appreciate is that in the healthy cells you have a nicely organized contractile apparatus with these dark black z discs eye bands and a band structures whereas in the dmd cells what we see are mostly aligned myofibrils so you can see some some of that and some degree of organization so you see some remnants of banding patterns but not to the level that's seen in the healthy tissues and so then if we stimulate those dmd tissues to undergo a series of twitch and tetanus contractions and then conduct our electron microscopy we find that in the case of a stimulated contraction that contractile apparatus shows up as just being scattered in all directions and is beyond repair so this then creates a perfect starting place for a contractile assay where then we're in a position to test treatments for the ability to both improve contractile apparatus maturation and to withstand the stress of induced contractions and so here again we're treating those dmd micro tissues with either an igg4 treatment or a beta one integrand activating antibody and then we go on to induce a series of twitch and tetanus contractions on day eight of culture followed by em analysis and hopefully what you can appreciate is um in this igg4 treatment we see that once again the sarcomeres are kind of spread all over the place but downstream of this beta one integrand activating treatment in these cells that lack dystrophin not only do we see that the contractile apparatus has withstand withstood the contraction but the organization of the sarcomere is starting to look very very similar to the healthy controls we see these dark z discs we still have the eye bands and the a bands so with that hopefully i have convinced you of the merits of enlisting 3d muscle cultures as a humanized pre-clinical setting to test the effects of promising therapeutics and assays of tissue function and as i mentioned i really truly believe that these assays could offer a powerful strategy in the quality control of myogenic cell products and also in evaluating the functional effects of promising gene therapies and rather than going into that in detail end here so we have a little time for discussion and perhaps we can talk about that during the discussion period all right thank you so much penny and thank you to all of our presenters for keeping us more or less on time challenging with these short slots um so we can now uh go through a couple questions there's there's some in the the q a box here and i would encourage our attendees to send any others along that that you would like answered uh we'll start with one for mod which is what makes hla matching less stringent when derived from cord blood so the current theory is really that uh the immune cells contained in i don't think you can see me anymore but i think you can hear me got some problems with my camera sorry um the immune cells contained within cord blood units are more immature than what you find in an adult and this leads to more tolerance against actually mismatches because the t cells are less mature less educated or selected there also might be another contribution um of the low low t cell those basically uh that are contained within the coordinate graphs so when compared to to what a patient would receive with bone marrow or peripheral blood um transplantation uh i think the the amount of t cells that they will receive is a hundred fold lower um which might also um uh decrease the the risk of graft versus source disease um so yeah basically that's that's the the reason why corbett is more tolerant for each of a mismatch in a gist okay great thank you so much uh this is a question for uh ronnie how long does the flag treatment last and from a therapeutic perspective would it be a one-time dose or continued uh administration yeah so it's a very good question actually the the flag are uh antibody based agonists so the half-life of the flag is uh similar or even better in vivo compared to igg which is around 20-30 days but and in term of the therapeutic perspective and patience like we know that before the t-span 12 knockout we were injecting every two days the mice but this is was ip injection for the oir model we were doing intravitreal injection one time so we don't know exactly like in a therapeutic perspective if it's one injector or multiple injection we hope that's gonna be one rejection because comparing to the anti-vgf where it's very aggressive you have to go like three four times per year in order to get the anti-vgf we don't know exactly i think but uh hopefully it's going to be like a better and we hope that it's only one application but we'll see okay fair enough thank you okay and a question for penny this is just a question out of curiosity from me um you know with these types of of models like the the beautiful one that that you've been developing um i guess there's always a question about how is the architecture affecting the cells you know is there anything specific that's coming from the interaction um of kind of the the template that you're putting the cells in have you guys looked at that at all the level of gene expression or just any other maybe even phenotypic properties do you mean in terms of the culture platforms themselves or the extracellular matrix compositions that are used as scaffolds yeah i was thinking of the the way that you're doing culture kind of as opposed to just cells in a regular old dish yeah so i think um at least from our standpoint the biggest difference between just sticking muscle cells in a culture dish and putting them in 3d cultures now you have ligation of the receptors on both the apical and the basal side and you have a system that allows the cells to contract and those contractions to be maintained and we know that those contractions are then translating to signal transduction in the cells which potentiates the maturation of the cells and ultimately that seems to be the key to ultimately making a muscle cell that has a higher degree of contractile apparatus maturation compared to what you're going to see in a 2d culture dish so it's just the types of questions you would ask in the two settings are just different sure if you can ask it in a 2d culture dish you should um it's not until you get to the point where you need to look at later stages of function that it makes sense to move to a 3d setting yeah okay makes sense thank you okay we have another question for mod is xlthera looking at applications for um 171 beyond cord blood expansion maybe to other engineered cell products so we're currently trying to transpose our technology to adult stem cells basically so um we know that there are um some some patients who need an autologous transplant and and some of them will will be what we call poor mobilizers so the number of stem cells that you can collect from these patients is very low um making it very risky to go through full transplant procedures with them and so expansion of these cells might also be an interesting um clinical use of the um 171 molecules um yeah that's that's the next step uh for us okay okay and there's one other question for you uh about the mechanism of action for um-171 are you allowed to talk about that at all yeah there was recently a paper published um i think it was in in cell stem cell by the vaginal lab basically describing a novel column 3 e3 ligase complex which was crucial for the the action of um 171 and basically regulating the epigenetic epigenetic signatures sorry um uh which are crucial for the maintenance of stem cells in vitro so um the paper is by jalila chagra i invite you to go read it and if you have any questions you you can always uh reach out to us uh will be it will be a pleasure for us to to answer your questions okay wonderful well those are the the questions so what we'll do now is take a very brief break three minutes and then we will be back with our next round of speakers but thanks so much to each of you for spending the time with us today these were just fantastic presentations really exciting science so thanks again and all of our attendees just uh stick with us and we'll be back in three minutes with the next round thank you so much thanks thank you all right well it's two o'clock so i think we should start things back up here we've got a great set of uh speakers for our next session and we're gonna start with sam wadsworth sam is the chief scientific officer and co-founder of aspect biosystems he earned a phd in respiratory cell biology from the university of nottingham he spent two decades driving developments in human tissue engineering in 2013 he co-founded ubc spit-out aspect biosystems with conrad wallace simon baer and tamara mohammed and aspect biosystems as you'll hear more about today is a biotech company creating bio-printed therapeutics as medicines of the future sam is going to tell us about aspects proprietary bioprinting technology and we'll talk about how it has the potential to revolutionize the field of regenerative medicine by enabling a new generation of allogeneic cell therapies so sam will turn it over to you i think you may just have one more button to click so that we have your slides kind of in in there you go perfect take it away great uh can you hear me okay shayna yes perfect uh well thanks for the introduction and thank you to medicine by design and the prime organizers of today's cell and gene therapies meeting thanks for the opportunity to present and i'm looking forward to updating you on the exciting progress that we've been making at aspect in creating bio-printed cellular therapeutics so um just to kind of summarize what we're trying to do here at aspect we're really focused on marrying our unique microfluidic bioprinting technology and manufacturing platform with advanced cell biology and biomaterials to generate bioprinted therapeutics and these are really we think the next generation of implantable cell-based therapeutics that we believe will unlock this next generation of cell therapies so a bit of background on aspect biosystems we span out from the university of british columbia in vancouver in late 2013 and it was really through a collaboration between two world-class research groups in medicine and engineering since we left campus and started to really ramp up commercial operations in around 2016 we've hit several key milestones we assembled a world-class research team with over 50 scientists based mainly here in vancouver scientists engineers and entrepreneurs we've built a strong intellectual property portfolio we have over 50 filings around the world we've created strategic partnerships with some of the biggest names in the industry and we're now leveraging our bioprinting platform to create our own proprietary pipeline of bioprinted therapeutics and so what is our technology well at the core of our technology is our microfluidic bioprinting platform and so we're the first and only company in the world that has really married the technologies of microfluidics and 3d printing and what this does is it allows us to really have an unprecedented level of control over the materials that we're able to print with with our pro with our platform we can integrate process and print multiple different bio materials that are loaded with therapeutically relevant cells and the way that we we print really enables us to print with really quite fragile cells so we are able to generate tissues that have very high cell viability um we can print with stem cells primary cells either individual cells or clusters and we can print with very high viability and this is because the levels of shear stress that the cells are exposed to is very low we're also able to not just switch between materials but also combine multiple materials and multiple different cell types in the same fiber as we as we generate our printed tissue and so we have very fine control over the positioning of cells and materials within our tissues at the fiber level and so what you see on this slide is really an illustration of one of our print heads i'm probably very small on the screen but you can see i'm holding in my hand one of our microfluidic printheads they're about the size of a usb stick they have multiple channels in the print head and what you see in this video here if i can get it started um is just an illustration and a video of how the different materials are routed through the printhead and combined into a single extrusion channel and we're able to switch between multiple different biomaterials and extrude a cell loaded fiber but this is a 3d printing technology and so we're able to pattern those cell loaded fibers into 3d macro structures and it's these macro structures that are our implantable cellular therapeutic tissues so really what we see is that um the ability to take a cell loaded fiber that has multiple layers within the fiber can enable us to really develop allogeneic cell therapies and this is because obviously if you have an allergenic cell it will be exposed to immune attack by the host after it's implanted into the patient and so what we use here is we're leveraging our ability to generate multi-layered fibers these fibers are only about the width of a human hair the cells are embedded within the core of the fiber and we have an outer shell that is a cell-free permeable membrane and that permeable material enables the influx of growth factors and oxygen to the cells in the center of the fiber and keeps those cells alive but it also provides protection from the adaptive immune system and so the cells are protected from immune attack and so this is really the the fundamental technology that we're using to generate allogeneic cell-based therapeutics importantly the patterns that we generate enable us to have consistent device function and also enable us to not just implant these devices but also go back in to the patient and potentially retrieve the devices as well now this kind of allergen excel bioprinted cell therapy platform is potentially applicable to multiple different diseases we have our own therapeutic pipeline that we're working on in-house and our initial area of focus is pancreatic tissue for the treatment of type 1 diabetes this is basically where we're encapsulating pancreatic islets or beta cells into these core shell devices and using those as a treatment developing these as a treatment for type 1 diabetes we also have liver tissues in development at a slightly earlier stage but again these are designed around the concept of printing and encapsulating hepatocytes for the treatment of various different liver diseases including acute liver failure and more chronic liver diseases as well we also have several discovery programs in early stages of development as well but today i'd like to talk about really the diabetes program that we have and focus in on some of the data that we're generating with this particular tissue and so the we've done a variety of in vitro experiments to demonstrate compatibility of our printing technology with pancreatic eyelids but i'm going to show you some in vivo data sets that we've generated more recently so what we do is as i said before we take these therapeutic cells in this case it's primary human pancreatic islets they're embedded in the core of a core shell fiber this fibers are about a millimeter in diameter these fibers are in this case they're eight centimeters long we place them into the intraperitoneal cavity of of mice these are immune deficient mice in this case and then after 31 days we retrieve the fibers stain them for live cells and we can see that the green staining shows that there is very high cell viability each of those green circles is a a pancreatic islet that shows high viability the red stain shows insulin positivity via dithizone stain and so these islets are also packed full of insulin and presumably quite functional even after 31 days in vivo the next experiment here was to test these tissues in diabetic models and so we took these immune deficient nsg mice and treated them with streptozotes in and you can see the trace on the bottom left of this slide shows blood glucose over time we see a spike in blood glucose as the animals become hyperglycemic after sdz treatment at zero days we implant with these eight centimeter long fibers into the ip cavity that contain the primary human eyelids and we get pretty rapid normalization of blood glucose and that's maintained out for around three months in vivo when the experiment was terminated this was multiple different uh donors of pancreatic eyelids and so we're confident that it's a a consistent effect this normalization of blood glucose is accompanied by a rise in human c-peptide as a surrogate for human insulin in these animals uh and then on the right hand side you can see the kinetics of response so this is where we give the animals a oral bolus of glucose the black line shows the control animals that are non-diabetic and you see a rapid spike in blood glucose that then normalizes fairly quickly the dotted blue line is the animals that were diabetic that received the human tissues and again we see a very similar kinetics of response with the implanted human tissues suggesting that the kinetics of the insulin release and subsequent control of glucose is physiologically appropriate in these animals now a single fiber may be enough to control blood glucose in a mouse but if we scale up to a human size um a fiber may need to be tens or hundreds of meters in length in order to load enough cells to control glucose and so what we are doing is taking those fibers and patterning them into the 3d structures that i described earlier and so on this slide what you see is this is some in vitro data demonstrating how we can take a fiber that's a much longer length we can pattern that into a 3d structure and the cells within that structure these are again primary human eyelets the cells are viable for several days post printing in vitro and then we perform functional assays glucose stimulated insulin secretion assays you see on the bottom right of the slide this is where we take those printed tissues and we treat them with different concentrations of glucose we go low high low and we see a corresponding increase and then return to baseline in secreted c peptide levels from these devices the amount of c-peptide that we see that's released is proportional to the number of cells that we incorporate in the device and it's almost a one-to-one ratio so if we double the number of cells that are in the devices we double the amount of c-peptide that's released and that's shown in the graph on the bottom right so this is how we're planning on scaling up the size of the device to human patients but we also want to scale out and so it's difficult to scale out using primary human islets the number of donors is is limited and so we're also collaborating with a group at ubc this is with tim kiefer's lab to basically access stem cell derived beta cells and this is some data showing in vitro functionality again using a gesis assay of bioprinted stem cell derived beta cells and then on the right hand side you can see a increase in circulating c peptide when we implant these stem cell containing tissues into animals and and so we get increase in functionality over time in vivo these experiments are ongoing and so to kind of bring this back together our goals as a company obviously is is to bring together our biomanufacturing our bioprinting technology with cells and biomaterials to generate these implanted 3d devices that come act as therapeutic tissues we're demonstrating some really good functionality of these in in vivo models in small animals and we're moving into larger animal models very soon [Music] we also have a broad range of of collaborators around the world through what we call our discovery ecosystem and this is where we place our bio printers into the labs of of experts and we work in various different tissue types not just the pancreas and the liver tissues that i described and so i'd be very happy to talk to people who are interested in working with us and collaborating if you have a goal of developing cell-based therapeutics and you think bioprinting could help then we'd be more than happy to talk to you please check out our website for more details and then just at the end i'd like to recognize the team that's behind all of this we have a large varied team here at aspect it's very exciting place to work and we have multiple different uh open positions that we're hiring for at the moment so again if you're interested in learning more about potentially helping us to develop these life-changing therapeutics please just reach out on our website or to me and i'd be happy to talk to you about this with that thanks very much and i'm happy to answer questions in the q a period later thank you so much sam that was fantastic really exciting so we'll come back to you for some questions at the end uh next we are going to move on to maria abdulkatra she's a trained biologist with a phd in computational and mathematical biology from mcmaster uh she was a postdoc at the max planck institute for evolutionary biology in germany and she is currently a research associate in the lab of gary bader who's in the donnelly center at the university of toronto she's been with us since 2016 and she's going to tell us more about her work developing 3d mathematical models that explore self-development go ahead maria thank you i'm just gonna start by sharing my screen you can see my screen now right yeah but i think you just need to click maybe to swap the displays which is that you see my like where my mouse is moving we see the like the presenter mode we don't see the full screen i'm sorry i'll do that again so there you go perfect sorry about that and uh hi everyone thank you um medicine by design and prime for the invitation and of course giving me the opportunity to talk about our work today um so i thought i'd start with a vision at least my vision and the possibility for a future where you can think of a patient can start and activate a specific treatment with just a simple push of a button or a thumbprint and this vision involves what others are calling the digital twin so it's a virtual proxy that can be used to analyze and test precise drugs regimes as an example this is of course a vision but we have the building blocks already in place for a future with such possibilities we have the experimental tools data and artificial intelligence already exchanging information and setting up the platform for learning and making these predictions however in my opinion we are still missing one of the more one another important building block and that is the mechanistic models models that use mathematical and physical sciences these models can help provide orthogonal information that may direct our decisions and perspectives they can even act as proxies to experiments and help us push boundaries outside of the accessible zone so i think by working together and tackle problems using these various tools we can forge new discoveries and maybe make way for this digital twin obviously i have no idea when we will get close to our digital twin but what i can tell you today is that we are close to what you can call the digital organoid or digital cell culture right now so you can add a virtual version of these tools and this can change maybe the way experiments are developed in designs models can guide the experiment and and can make initial predictions before you start so to develop um these virtual cells we start by integrating knowledge from many disciplines and as a platform it is powerful modelable and fast for example here i'm i'm showing just a platform where we chose a time as developmental days you can have death probability density and any other cues that were associated with cell behavior and cell decisions this is what we call rule-based agent models the rules can be explored individually or in combination and the rules we apply in the model they can help generate emergent behaviors so these help make predictions we can track lineages across 3d space and time and all all this is done at any resolution so in this case it's the single cell level so we can then apply the same analysis that is done on the current single cell experiments for instance basically creative the creativity lies in figuring out how to translate our knowledge from text to algorithm and then to decide what to include and exclude in the system but what happens when we ask a question and there is no answer or there is a gap in our knowledge this is where models can also do more than just make predictions they can help fill missing information this is this was the case when we started building the model that aims to disentangle how a single cell generates a diversity needed to create a living organism we started integrating the algorithm the algorithm that captures cell division because development pretty much starts with a lot
2021-07-25