Mark Zuckerberg & Dr. Priscilla Chan: Curing All Human Diseases & the Future of Health & Technology
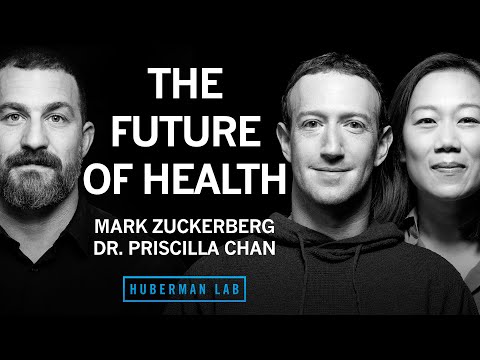
ANDREW HUBERMAN: Welcome to the Huberman Lab podcast, where we discuss science and science-based tools for everyday life. [MUSIC PLAYING] I'm Andrew Huberman. And I'm a professor of neurobiology and ophthalmology at Stanford School of Medicine.
My guests today are Mark Zuckerberg and Dr. Priscilla Chan. Mark Zuckerberg, as everybody knows, founded the company Facebook. He is now the CEO of Meta, which includes Facebook, Instagram, WhatsApp, and other technology platforms. Dr. Priscilla Chan graduated from Harvard
and went on to do her medical degree at the University of California San Francisco. Mark Zuckerberg and Dr. Priscilla Chan are married and the co-founders of the CZI, or Chan Zuckerberg Initiative, a philanthropic organization whose stated goal is to cure all human diseases. The Chan Zuckerberg Initiative is accomplishing that by providing critical funding not available elsewhere, as well as a novel framework for discovery of the basic functioning of cells, cataloging all the different human cell types, as well as providing AI, or artificial intelligence, platforms to mine all of that data to discover new pathways and cures for all human diseases. The first hour of today's discussion is held with both Dr. Priscilla Chan and Mark Zuckerberg,
during which we discuss the CZI and what it really means to try and cure all human diseases. We talk about the motivational backbone for the CZI that extends well into each of their personal histories. Indeed, you'll learn quite a lot about Dr. Priscilla Chan, who has, I must say, an absolutely incredible family story leading up to her role as a physician and her motivations for the CZI and beyond. And you'll learn from Mark, how he is bringing an engineering and AI perspective to the discovery of new cures for human disease.
The second half of today's discussion is just between Mark Zuckerberg and me, during which we discuss various Meta Platforms, including, of course, social media platforms, and their effects on mental health in children and adults. We also discuss VR, Virtual Reality, as well as augmented and mixed reality. And we discuss AI, Artificial Intelligence, and how it stands to transform not just our online experiences with social media and other technologies, but how it stands to potentially transform every aspect of everyday life. Before we begin, I'd like to emphasize that this podcast is separate from my teaching and research roles at Stanford. It is, however, part of my desire and effort to bring zero cost to consumer information about science and science-related tools to the general public. In keeping with that theme, I'd like to thank the sponsors of today's podcast.
Our first sponsor is Eight Sleep Eight Sleep makes smart mattress covers with cooling, heating, and sleep tracking capacity. I've spoken many times before on this podcast about the fact that getting a great night's sleep really is the foundation of mental health, physical health and performance. One of the key things to getting a great night's sleep is to make sure that the temperature of your sleeping environment is correct. And that's because in order to fall and stay deeply asleep, your body temperature actually has to drop by about 1 to 3 degrees.
And in order to wake up feeling refreshed and energized, your body temperature actually has to increase by about 1 to 3 degrees. With Eight Sleep, you can program the temperature of your sleeping environment in the beginning, middle, and end of your night. It has a number of other features, like tracking the amount of rapid eye movement and slow wave sleep that you get, things that are essential to really dialing in the perfect night's sleep for you. I've been sleeping on an Eight Sleep mattress cover for well over two years now. And it has greatly improved my sleep.
I fall asleep far more quickly. I wake up far less often in the middle of the night. And I wake up feeling far more refreshed than I ever did prior to using an Eight Sleep mattress cover. If you'd like to try Eight Sleep, you can go to eightsleep.com/huberman to save
$150 off their Pod 3 cover. Eight Sleep currently ships to the USA, Canada, UK, select countries in the EU, and Australia. Again, that's eightsleep.com/huberman. Today's episode is also brought to us by LMNT. LMNT is an electrolyte drink that has everything you need and nothing you don't. That means plenty of electrolytes-- sodium, magnesium and potassium-- and no sugar.
The electrolytes are absolutely essential for the functioning of every cell in your body. And your neurons, your nerve cells, rely on sodium, magnesium and potassium in order to communicate with one another electrically and chemically. LMNT contains the optimal ratio of electrolytes for the functioning of neurons and the other cells of your body. Every morning, I drink a packet of LMNT dissolved in about 32 ounces of water. I do that just for general hydration and to make sure that I have adequate electrolytes for any activities that day. I'll often also have an LMNT packet, or even two packets, in 32 to 60 ounces of water if I'm exercising very hard and certainly if I'm sweating a lot, in order to make sure that I replace those electrolytes.
If you'd like to try LMNT, you can go to drinklmnt.com/huberman to get a free sample pack with your purchase. Again, that's drinklmnt.com/huberman. I'm pleased to announce that we will be hosting four live events in Australia, each of which is entitled The Brain Body Contract, during which I will share science and science-related tools for mental health, physical health, and performance.
There will also be a live question and answer session. We have limited tickets still available for the event in Melbourne on February 10, as well as the event in Brisbane on February 24. Our event in Sydney, at the Sydney Opera House, sold out very quickly. So as a consequence, we've now scheduled a second event in Sydney at the Aware Super Theatre on February 18. To access tickets to any of these events, you can go to hubermanlab.com/events and use the code Huberman at checkout.
I hope to see you there. And as always, thank you for your interest in science. And now, for my discussion with Mark Zuckerberg and Dr. Priscilla Chan.
Priscilla, Mark, so great to meet you. And thank you for having me here in your home. MARK ZUCKERBERG: Oh, Thanks for having us on the podcast. PRISCILLA CHAN: Yeah.
ANDREW HUBERMAN: I'd like to talk about the CZI, the Chan Zuckerberg Initiative. I learned about this a few years ago, when my lab was-- and still is now-- at Stanford, as a very exciting philanthropic effort that has a truly big mission. I can't imagine a bigger mission.
So maybe you could tell us what that big mission is. And then we can get into some of the mechanics of how that big mission can become a reality. PRISCILLA CHAN: So like you're mentioning, in 2015, we launched the Chan Zuckerberg Initiative.
And what we were hoping to do at CZI was think about how do we build a better future for everyone and looking for ways where we can contribute the resources that we have to bring philanthropically and the experiences that Mark and I have had, for me as a physician and educator, for Mark as an engineer, and then our ability to bring teams together to build the builders. Mark has been a builder throughout his career. And what could we do if we actually put together a team to build tools, do great science? And so within our science portfolio, we've really been focused on what some people think is either an incredibly audacious goal or an inevitable goal. But I think about it as something that will happen if we continue focusing on it, which is to be able to cure, prevent, or manage all disease by the end of the century.
ANDREW HUBERMAN: All disease? PRISCILLA CHAN: All disease. So that's important, right? And so a lot of times, people ask like, which disease? And the whole point is that there is not one disease. And it's really about taking a step back to where I always found the most hope as a physician, which is new discoveries and new opportunities and new ways of understanding how to keep people well come from basic science. So our strategy at CZI is really to build tools, fund science, change the way basic scientists can see the world and how they can move quickly in their discoveries. And so that's what we launched in 2015.
We do work in three ways. We fund great scientists. We build tools-- right now, software tools to help move science along and make it easier for scientists to do their work. And we do science.
You mentioned Stanford being an important pillar for our science work. We've built what we call biohubs, institutes where teams can take on grand challenges to do work that wouldn't be possible in a single lab or within a single discipline. And our first biohub was launched in San Francisco, a collaboration between Stanford, UC Berkeley, and UCSF. ANDREW HUBERMAN: Amazing.
Curing all diseases implies that there will either be a ton of knowledge gleaned from this effort, which I'm certain there will be-- and there already has been. We can talk about some of those early successes in a moment. But it also sort of implies that if we can understand some basic operations of diseases and cells that transcend autism, Huntington's, Parkinson's, cancer and any other disease that perhaps there are some core principles that would make the big mission a real reality, so to speak.
What I'm basically saying is, how are you attacking this? My belief is that the cell sits at the center of all discussion about disease, given that our body is made up of cells and different types of cells. So maybe you could just illuminate for us a little bit of what the cell is, in your mind, as it relates to disease and how one goes about understanding disease in the context of cells because, ultimately, that's what we're made up of. MARK ZUCKERBERG: Yeah.
Well, let's get to the cell thing in a moment. But just even taking a step back from that, we don't think, at CZI, that we're going to cure, prevent or manage all diseases. The goal is to basically give the scientific community and scientists around the world the tools to accelerate the pace of science. And we spent a lot of time, when we were getting started with this, looking at the history of science and trying to understand the trends and how they've played out over time. And if you look over this very long-term arc, most large-scale discoveries are preceded by the invention of a new tool or a new way to see something.
And it's not just in biology, right? It's like having a telescope came before a lot of discoveries in astronomy and astrophysics. But similarly, the microscope and just different ways to observe things or different platforms, like the ability to do vaccines preceded the ability to cure a lot of different things. So this is the engineering part that you were talking about, about building tools. We view our goal is to try to bring together some scientific and engineering knowledge to build tools that empower the whole field. And that's the big arc and a lot of the things that we're focused on, including the work in single cell and cell understanding, which you can jump in and get into that if you want. But yeah, I think I think we generally agree with the premise that if you want to understand this stuff from first principles-- people study organs a lot right.
You study how things present across the body. But there's not a very widespread understanding of how each cell operates. And this is a big part of some of the initial work that we tried to do on the Human Cell Atlas and understanding what are the different cells. And there's a bunch more work that we want to do to carry that forward. But overall, I think, when we think about the next 10 years here of this long arc to try to empower the community to be able to cure, prevent or manage all diseases, we think that the next 10 years should really be primarily about being able to measure and observe more things in human biology.
There are a lot of limits to that. It's like you want to look at something through a microscope, you can't usually see living tissues because it's hard to see through skin or things like that. So there are a lot of different techniques that will help us observe different things. And this is where the engineering background comes in a bit because-- I mean, when I think about this is from the perspective of how you'd write code or something, the idea of trying to debug or fix a code base, but not be able to step through the code line by line, it's not going to happen, right? And at the beginning of any big project that we do at Meta, we like to spend a bunch of the time up front just trying to instrument things and understand what are we going to look at and how are we going to measure things so we know we're making progress and know what to optimize. And this is such a long-term journey that we think that it actually makes sense to take the next 10 years to build those kinds of tools for biology and understanding just how the human body works in action. And a big part of that is, cells.
I don't know. Do you want to jump and talk about some of the efforts? PRISCILLA CHAN: Sure. ANDREW HUBERMAN: Could I just interrupt briefly and just ask about the different interventions, so to speak, that CZI is in a unique position to bring to the quest to cure all diseases? So I can think of-- I mean, I know, as a scientist, that money is necessary but not sufficient, right? When you have money, you can hire more people. You can try different things. So that's critical.
But a lot of philanthropy includes money. The other component is you want to be able to see things, as you pointed out. So you want to know that normal disease process-- like, what is a healthy cell? What's a diseased cell? Are cells constantly being bombarded with challenges and then repairing those? And then what we call cancer is just a runaway train of those challenges not being met by the cell itself or something like that? So better imaging tools. And then it sounds like there's not just a hardware component, but a software component. This is where AI comes in. So maybe, at some point, we can break this up into two, three different avenues.
One is understanding disease processes and healthy processes. We'll lump those together. Then there's hardware-- so microscopes, lenses, digital deconvolution, ways of seeing things in bolder relief and more precision. And then there's how to manage all the data. And then I love the idea that maybe AI could do what human brains can't do alone, like manage understanding of the data because it's one thing to organize data. It's another to say, oh, this as you point out in the analogy with code, that this particular gene and that particular gene are potentially interesting, whereas a human being would never make that potential connection.
MARK ZUCKERBERG: Yeah. PRISCILLA CHAN: So the tools that CZI can bring to the table-- we fund science, like you're talking about. There's lots of ways to fund science. And just to be clear, what we fund is a tiny fraction of what the NIH funds, for instance. ANDREW HUBERMAN: So you guys have been generous enough that it definitely holds wait to NIH's contribution.
PRISCILLA CHAN: Yeah. But I think every funder has its own role in the ecosystem. And for us, it's really, how do we incentivize new points of view? How do we incentivize collaboration? How do we incentivize open science? And so a lot of our grants include inviting people to look at different fields. Our first neuroscience RFA was aimed towards incentivizing people from different backgrounds-- immunologists, microbiologists-- to come and look at how our nervous system works and how to keep it healthy. Or we ask that our grantees participate in the pre-print movement to accelerate the rate of sharing knowledge and actually others being able to build upon science. So that's the funding that we do.
In terms of building, we build software and hardware, like you mentioned. We put together teams that can build tools that are more durable and scalable than someone in a single lab might be incentivized to do. There's a ton of great ideas. And nowadays, most scientists can tinker and build something useful for their lab. But it's really hard for them to be able to share that tool sometimes beyond their own laptop or forget the next Lab over or across the globe. So we partner with scientists to see what is useful, what kinds of tools.
In imaging, Napari, it's a useful image annotation tool that is born from an open source community. And how can we contribute to that? Or a CELLxGENE, which works on single cell data sets. And how can we make it build a useful tool so that scientists can share data sets, analyze their own and contribute to a larger corpus of information? So we have software teams that are building, collaborating with scientists to make sure that we're building easy to use, durable, translatable tools across the scientific community in the areas that we work in.
We also have institutes-- this is where the imaging work comes in-- where we are proud owners of an electron microscope right now. It's going to be installed at our imaging institute. And that will really contribute to the way where we can see work differently. But more hardware does need to be developed.
We're partnering with the fantastic scientists in the biohub network to build a mini-phase plate to increase to align the electrons through the electron microscope to be able to increase the resolution, so we can see in sharper detail. So there's a lot of innovative work within the network that's happening. And these institutes have grand challenges that they're working on. Back to your question about cells, cells are just the smallest unit that are alive. And your body, all of our bodies, have many, many, many cells. Some estimate of like 37 trillion cells, different cells in your body.
And what are they all doing? And what do they look like when you're healthy? What do they look like when you're sick? And where we're at right now with our understanding of cells and what happens when you get sick is basically we've gotten pretty good at, from the Human Genome Project, looking at how different mutations in your genetic code lead for you to be more susceptible to get sick or directly cause you to get sick. So we go from a mutation in your DNA to, wow, you now have Huntington's disease, for instance. And there's a lot that happens in the middle. And that's one of the questions that we're going after at CZI, is what actually happens. So an analogy that I like to use to share with my friends is, right now, say we have a recipe for a cake. We know there's a typo in the recipe.
And then the cake is awful. That's all we know. We don't know how the chef interprets the typo. We don't know what happens in the oven. And we don't actually know how it's exactly connected to how the cake didn't turn out or how you had expected it.
A lot of that is unknown. But we can actually systematically try to break this down. And one segment of that journey that we're looking at is how that mutation gets translated and acted upon in your cells. And all of your cells have what's called mRNA. mRNA are the actual instructions that are taken from the DNA.
And our work in Single-Cell is looking at how every cell in your body is actually interpreting your DNA slightly differently and what happens when healthy cells are interpreting the DNA instructions and when sick cells are interpreting those directions. And that is a ton of data. I just told you, there's 37 trillion cells. There's different large sets of mRNA in each cell. But the work that we've been funding is looking at how-- first of all, gathering that information. We've been incredibly lucky to be part of a very fast-moving field where we've gone from, in 2017, funding some methods work to now having really not complete, but nearly complete atlases of how the human body works, how flies work, how mice work at the single-cell level and being able to then try to piece together how does that all come together when you're healthy and when you're sick.
And the neat thing about the inflection point where we're at in AI is that I can't look at this data and make sense of it. There's just too much of it. And biology is complex. Human bodies are complex. We need this much information.
But the use of large language models can help us actually look at that data and gain insights, look at what trends are consistent with health and what trends are unsuspected. And eventually, our hope, through the use of these data sets that we've helped curate and the application of large language models, is to be able to formulate a virtual cell, a cell that's completely built off of the data sets of what we know about the human body, but allows us to manipulate, and learn faster and try new things to help move science and then medicine along. ANDREW HUBERMAN: Do you think we've cataloged the total number of different cell types? Every week, I look at great journals like Cell Nature and Science. And for instance, I saw recently that, using single cell sequencing, they've categorized 18 plus different types of fat cells. We always think of like a fat cell versus a muscle cell. So now, you've got 18 types.
Each one is going to express many, many different genes and mRNAs. And perhaps one of them is responsible for what we see in advanced type 2 diabetes, or in other forms of obesity, or where people can't lay down fat cells, which turns out to be just as detrimental in those extreme cases. So now, you've got all these lists of genes. But I always thought of single cell sequencing as necessary, but not sufficient, right? You need the information, but it doesn't resolve the problem. And I think of it more as a hypothesis-generating experiment. OK, so you have all these genes.
And you can say, well, this gene is particularly elevated in the diabetic cell type of, let's say, one of these fat cells or muscle cells for that matter, whereas it's not in non-diabetics. So then of the millions of different cells, maybe only five of them differ dramatically. So then you generate a hypothesis.
Oh, it's the ones that differ dramatically that are important. But maybe one of those genes, when it's only 50% changed, has a huge effect because of some network biology effect. And so I guess what I'm trying to get to here is how does one meet that challenge. And can AI help resolve that challenge by essentially placing those lists of genes into 10,000 hypotheses? Because I'll tell you that the graduate students and postdocs in my lab get a chance to test one hypothesis at a time. PRISCILLA CHAN: I know.
ANDREW HUBERMAN: And that's really the challenge, let alone one lab. And so for those that are listening to this-- and hopefully, it's not getting outside the scope of standard understanding or the understanding we've generated here. But what I'm basically saying is, you have to pick at some point. More data always sounds great. But then how do you decide what to test? PRISCILLA CHAN: So no, we don't know all the cell types.
I think one thing that was really exciting when we first launched this work was cystic fibrosis. Cystic fibrosis is caused by mutation in CFTR. That's pretty well known. It affects a certain channel that makes it hard for mucus to be cleared. That's the basics of cystic fibrosis. When I went to medical school, it was taught as fact.
ANDREW HUBERMAN: So their lungs fill up with fluid. These are people who are carrying around sacks of fluid filling up. PRISCILLA CHAN: Yep. ANDREW HUBERMAN: I've worked with people like that. And they have to literally dump the fluid out. PRISCILLA CHAN: Exactly.
ANDREW HUBERMAN: They can't run or do intense exercise. Life is shorter. PRISCILLA CHAN: Life is shorter.
And when we applied single-cell methodologies to the lungs, they discovered an entirely new cell type that actually is affected by a mutation in the CF mutation, in cystic fibrosis mutation, that actually changes the paradigm of how we think about cystic fibrosis. ANDREW HUBERMAN: Amazing. PRISCILLA CHAN: [? Just ?] [? unknown. ?] So I don't think we know all the cell types. I think we'll continue to discover them. And we'll continue to discover new relationships between cell and disease, which leads me to the second example I want to bring up, is this large data set that the entire scientific community has built around single cell.
It's starting to allow us to say this mutation, where is it expressed? What types of cell types it's expressed in? And we actually have built a tool at CZI called CELLxGENE, where you can put in the mutation that you're interested in. And it gives you a heat map of cross cell types of which cell types are expressing the gene that you're interested in. And so then you can start looking at, OK, if I look at gene X and I know it's related to heart disease-- but if you look at the heat map, it's also spiking in the pancreas. That allows you to generate a hypothesis. Why? And what happens when this gene is mutated and the function of your pancreas? Really exciting way to look and ask questions differently.
And you can also imagine a world where if you're trying to develop a therapy, a drug, and the goal is to treat the function in the heart, but you know that it's also really active in the pancreas again. So is there going to be an unexpected side effect that you should think about as you're bringing this drug to clinical trials? So it's an incredibly exciting tool and one that's only going to get better as we get more and more sophisticated ways to analyze the data. ANDREW HUBERMAN: I must say, I love that because if I look at the advances in neuroscience over the last 15 years, most of them didn't necessarily come from looking at the nervous system. They came from the understanding that the immune system impacts the brain. Everyone prior to that talked about the brain as an immune-privileged organ. What you just said also bridges the divide between single cells, organs and systems, right? Because ultimately, cells make up organs.
Organs make up systems. And they're all talking to one another. And everyone nowadays is familiar with gut-brain axis or the microbiome being so important. But rarely is the discussion between organs discussed, so to speak. So I think it's wonderful. So that tool was generated by CZI.
Or CCI funded that tool? MARK ZUCKERBERG: We built that. PRISCILLA CHAN: We built it. ANDREW HUBERMAN: You built it. So is it built by Meta? Is this Meta? MARK ZUCKERBERG: No, no, it has its own engineers. ANDREW HUBERMAN: Got it. MARK ZUCKERBERG: Yeah.
They're completely different organizations. ANDREW HUBERMAN: Incredible. And so a graduate student or postdoc who's interested in a particular mutation could put this mutation into this database. That graduate student or postdoc might be in a laboratory known for working on heart, but suddenly find that they're collaborating with other scientists that work on the pancreas, which also is wonderful because it bridges the divide between these fields. Fields are so siloed in science-- not just different buildings, but people rarely talk, unless things like this are happening.
PRISCILLA CHAN: I mean, the graduate student is someone that we want to empower because, one, they're the future of science, as you know. And within CELLxGENE, if you put in the gene you're interested in and it shows you the heat map, we also will pull up the most relevant papers to that gene. And so read these things.
ANDREW HUBERMAN: That's fantastic. As we all know, quality nutrition influences, of course, our physical health, but also our mental health and our cognitive functioning-- our memory, our ability to learn new things and to focus. And we know that one of the most important features of high quality nutrition is making sure that we get enough vitamins and minerals from high quality, unprocessed, or minimally processed sources, as well as enough probiotics, and prebiotics and fiber to support basically all the cellular functions in our body, including the gut microbiome. Now, I, like most everybody try to get optimal nutrition from whole foods, ideally mostly from minimally processed or non processed foods. However, one of the challenges that I and so many other people face is getting enough servings of high quality fruits and vegetables per day, as well as fiber and probiotics that often accompany those fruits and vegetables. That's why, way back in 2012, long before I ever had a podcast, I started drinking AG1.
And so I'm delighted that AG1 is sponsoring the Huberman Lab podcast. The reason I started taking AG1 and the reason I still drink AG1 once or twice a day is that it provides all of my foundational nutritional needs. That is, it provides insurance that I get the proper amounts of those vitamins, minerals, probiotics and fiber to ensure optimal mental health, physical health and performance. If you'd like to try AG1, you can go to drinkag1.com/huberman
to claim a special offer. They're giving away five free travel packs plus a year's supply of vitamin D3 K2. Again, that's drinkag1.com/huberman to claim that special offer. MARK ZUCKERBERG: I just think going back to your question from before are there going to be more cell types that get discovered? I mean, I assume so, right? I mean, no catalog of this stuff is ever-- it doesn't seem like we're ever done. we keep on finding more.
But I think that that gets to one of the things that I think are the strengths of modern LLMs, is the ability to imagine different states that things can be in. So from all the work that we've done and funded on the Human Cell Atlas, there is a large corpus of data that you can now train a kind of large-scale model on. And one of the things that we're doing at CZI, which I think is pretty exciting, is building what we think is one of the largest non-profit life sciences AI clusters.
It's on the order of 1,000 GPUs. And it's larger than what most people have access to in academia that you can do serious engineering work on. And by basically training a model with all of the Human Cell Atlas Data and a bunch of other inputs as well, we think you'll be able to basically imagine all of the different types of cells and all the different states that they can be in, and when they're healthy and diseased, and how they'll interact with different-- interact with each other, interact with different potential drugs. But I think the state of LLMs, I think this is where it's helpful to understand-- have a good understanding and be grounded in the modern state of AI. I mean, these things are not foolproof. I mean, one of the flaws of modern LLMs is they hallucinate.
So the question is, how do you make it so that that can be an advantage rather than a disadvantage? And I think the way that it ends up being an advantage is when they help you imagine a bunch of states that someone could be in, but then you, as the scientist or engineer, go and validate that those are true, whether they're solutions to how a protein can be folded or possible states that a cell could be in when it's interacting with other things. But we're not yet at the state with AI that you can just take the outputs of these things as gospel and run from there. But they are very good, I think as you said, hypothesis generators or possible solution generators that then you can go validate. So I think that that's a very powerful thing that we can basically-- building on the first five years of science work around the Human Cell Atlas and all the data that's been built out-- carry that forward into something that I think is going to be a very novel tool going forward. And that's the type of thing that I think we're set up to do well.
I mean, you had this exchange a little while back about funding levels and how CZI is just a drop in the bucket compared to NIH. The thing that I think we can do that's different is funding some of these longer term, bigger projects. It is hard to galvanize the and pull together the energy to do that. And it's a lot of what most science funding is, relatively small projects that are exploring things over relatively short time horizons. And one of the things that we try to do is build these tools over 5, 10, 15-year periods. They're often projects that require hundreds of millions of dollars of funding and world-class engineering teams and infrastructure to do.
And that, I think, is a pretty cool contribution to the field that I think is-- there aren't as many other folks who are doing that kind of thing. But that's one of the reasons why I'm personally excited about the virtual cell stuff because it just this perfect intersection of all the stuff that we've done in single cell, the previous collaborations that we've done with the field and bringing together the industry and AI expertise around this. ANDREW HUBERMAN: Yeah, I completely agree that the model of science that you're putting together with CZI isn't just unique from NIH, but it's extremely important that the independent investigator model is what's driven the progression of Science in this country and, to some extent, in Northern Europe for the last 100 years.
And it's wonderful, on the one hand, because it allows for that image we have of a scientist tinkering away or the people in their lab, and then the eurekas. And that hopefully translates to better human health. But I think, in my opinion, we've moved past that model as the most effective model or the only model that should be explored. MARK ZUCKERBERG: Yeah, I just think it's a balance.
You want that. But you want to empower those people. I think that that's these tools empower those folks.
ANDREW HUBERMAN: Sure. And there are mechanisms to do that, like NIH. But it's hard to do collaborative science. It's interesting that we're sitting here not far-- because I grew up right near here as well. I'm not far from the garage model of tech, right? The Hewlett-Packard model, not far from here at all.
And the idea was the tinkerer in the garage, the inventor. And then people often forget that to implement all the technologies they discovered took enormous factories and warehouses. So there's a similarity there to Facebook, Meta, et cetera.
But I think, in science, we imagine that the scientists alone in their laboratory and those eureka moments. But I think, nowadays, the big questions really require extensive collaboration and certainly tool development. And one of the tools that you keep coming back to is these LLMs, these large language models. And maybe you could just elaborate, for those that aren't familiar. What is a large language model? For the uninformed, what is it? And what does it allow us to do that different, other types of AI don't allow? Or more importantly, perhaps what does it allow us to do that a bunch of really smart people, highly informed in a given area of science, staring at the data-- what can it do that they can't do? MARK ZUCKERBERG: Sure. So I think a lot of the progression of machine learning has been about building systems, neural networks or otherwise, that can basically make sense and find patterns in larger and larger amounts of data.
And there was a breakthrough a number of years back that some folks at Google actually made called this transformer model architecture. And it was this huge breakthrough because before then there was somewhat of a cap where if you fed more data into a Neural Network past some point, it didn't really glean more insights from it, whereas transformers just-- we haven't seen the end of how big that can scale to yet. I mean, I think that there's a chance that we run into some ceiling. ANDREW HUBERMAN: So it never asymptotes? MARK ZUCKERBERG: We haven't observed it yet.
But we just haven't built big enough systems yet. So I would guess that-- I don't know. I think that this is actually one of the big questions in the AI field today, is basically, are transformers and are the current model architectures sufficient? If you just build larger and larger clusters, do you eventually get something that's like human intelligence or super intelligence? Or is there some kind of fundamental limit to this architecture that we just haven't reached yet? And once we get a little bit further in building them out, then we'll reach that. And then we'll need a few more leaps before we get to the level of AI that I think will unlock a ton of really futuristic and amazing things.
But there's no doubt that even just being able to process the amount of data that we can now with this model architecture has unlocked a lot of new use cases. And the reason why they're called large language models is because one of the first uses of them is people basically feed in all of the language from, basically, the world wide web. And you can think about them as basically prediction machines. You put in a prompt. And it can basically predict a version of what should come next.
So you type in a headline for a news story. And it can predict what it thinks the story should be. Or you could train it so that it could be a chat, bot where, OK, if you're prompted with this question, you, can get this response. But one of the interesting things is it turns out that there's actually nothing specific to using human language in it.
So if instead of feeding it human language, if you use that model architecture for a network and instead you feed it all of the Human Cell Atlas Data, then if you prompt it with a state of a cell, it can spit out different versions of how that cell can interact or different states that the cell could be in next when it interacts with different things. ANDREW HUBERMAN: Does it have to take a genetics class? So for instance, if you give it a bunch of genetics data, do you have to say, hey, by the way, and then you give it a genetics class so it understands that you've got DNA, RNA, mRNA, and proteins? MARK ZUCKERBERG: No, I think that the basic nature of all these machine learning techniques is they're basically pattern recognition systems. So there are these very deep statistical machines that are very efficient at finding patterns. So it's not actually-- you don't need to teach a language model that's trying to speak a language a lot of specific things about that language either. You just feed it in a bunch of examples.
And then let's say you teach it about something in English, but then you also give it a bunch of examples of people speaking Italian. It'll actually be able to explain the thing that it learned in English in Italian. So the crossover and just the pattern recognition is the thing that is pretty profound and powerful about this. But it really does apply to a lot of different things. Another example in the scientific community has been the work that AlphaFold, basically the folks at DeepMind, have done on protein folding.
It's just basically a lot of the same model architecture. But instead of language, there they fold they fed in all of these protein data. And you can give it a state. And it can spit out solutions to how those proteins get folded.
So it's very powerful. I don't think we know yet, as an industry, what the natural limits of it are. I think that that's one of the things that's pretty exciting about the current state.
But it's certainly allows you to solve problems that just weren't solved with the generation of machine learning that came before it. ANDREW HUBERMAN: It sounds like CZI is moving a lot of work that was just done in vitro, in dishes, and in vivo, in living organisms, model organisms are humans, to in silico, as we say. So do you foresee a future where a lot of biomedical research, certainly the work of CZI included, is done by machines? I mean, obviously, it's much lower cost. And you can run millions of experiments, which, of course, is not to say that humans are not going to be involved.
But I love the idea that we can run experiments in silico en masse. PRISCILLA CHAN: I think in silico experiments are going to be incredibly helpful to test things quickly, cheaply and just unleash a lot of creativity. I do think you need to be very careful about making sure it still translates and matches the humans. One thing that's funny in basic science is we've basically cured every single disease in mice.
We know what's going on when they have a number of diseases because they're used as a model organism. But they are not humans. And a lot of times, that research is relevant, but not directly one-to-one translatable to humans. So you just have to be really careful about making sure that it actually works for humans. ANDREW HUBERMAN: Sounds like what CZI is doing is actually creating a new field.
As I'm hearing all of this, I'm thinking, OK, this transcends immunology department, cardiothoracic surgery, I mean neuroscience. I mean, the idea of a new field, where you certainly embrace the realities of universities and laboratories because that's where most of the work that you're funding is done. Is that right? MARK ZUCKERBERG: Mm-hmm. ANDREW HUBERMAN: So maybe we need to think about what it means to do science differently. And I think that's one of the things that's most exciting.
Along those lines, it seems that bringing together a lot of different types of people at different major institutions is going to be especially important. So I know that the initial CZI Biohub, gratefully, included Stanford. We'll put that first in the list, but also UCSF, forgive me. I have many friends at UCSF and also Berkeley. But there are now some additional institutions involved.
So maybe you could talk about that, and what motivated the decision to branch outside the Bay Area and why you selected those particular additional institutions to be included. MARK ZUCKERBERG: Well, I'll just say it. A big part of why we wanted to create additional biohubs is we were just so impressed by the work that the folks who were running the first biohub did. PRISCILLA CHAN: Yeah. And you should walk through the work of the Chicago Biohub and the New York Biohub that we just announced. But I think it's actually an interesting set of examples that balance the limits of what you want to do with physical material engineering and where things are purely biological because the Chicago team is really building more sensors to be able to understand what's going on in your body.
But that's more of a physical kind of engineering challenge, whereas the New York team-- we basically talk about this as like a cellular endoscope of being able to have an immune cell or something that can go and understand, what's the thing that's going on in your body? But it's not a physical piece of hardware. It's a cell that you can basically have just go report out on different things that are happening inside the body. ANDREW HUBERMAN: Oh, so making the cell the the microscope.
PRISCILLA CHAN: Totally. MARK ZUCKERBERG: And then eventually actually being able to act on it. But I mean, you should go into more detail on all this.
PRISCILLA CHAN: So a core principle of how we think about biohubs is that it has to be-- when we invited proposals, it has to be at least three institutions, so really breaking down the barrier of a single university, oftentimes asking for the people designing the research aim to come from all different backgrounds and to explain why that the problem that they want to solve requires interdisciplinary, inter-university, institution collaboration to actually make happen. We just put that request for proposal out there with our San Francisco Biohub as an example, where they've done incredible work in single cell biology and infectious disease. And we got-- I want to say-- like 57 proposals from over 150 institutions. A lot of ideas came together. And we were so, so excited that we've been able to launch Chicago and New York. Chicago is a collaboration between UIUC, University of Illinois Urbana-Champaign, and University of Chicago and Northwestern.
Obviously, these universities are multifaceted. But if I were to describe them by their stereotypical strength, Northwestern has an incredible medical system and hospital system. University of Chicago brings to the table incredible basic science strengths. University of Illinois is a computing powerhouse. And so they came together and proposed that they were going to start thinking about cells in tissue, so one of the layers that you just alluded to. So how do the cells that we know behave and act differently when they come together as a tissue? And one of the first tissues that they're starting with is skin.
So they've already been able to, as a collaboration under the leadership, of Shana Kelly design engineered skin tissue. The architecture looks the same as what's in you and I. And what they've done is built these super, super thin sensors. And they embed these sensors throughout the layers of this engineered tissue. And they read out the data. They want to see what these cells are secreting, how these cells talk to each other and what happens when these cells get inflamed.
Inflammation is an incredibly important process that drives 50% of all deaths. And so this is another disease-agnostic approach. We want to understand inflammation. And they're going to get a ton of information out from these sensors that tell you what happens when something goes awry because right now we can say, when you have an allergic reaction, your skin gets red and puffy. But what is the earliest signal of that? And these sensors can look at the behaviors of these cells over time.
And then you can apply a large language model to look at the earliest statistically significant changes that can allow you to intervene as early as possible. So that's what Chicago's doing. They're starting in the skin cells. They're also looking at the neuromuscular junction, which is the connection between where a neuron attaches to a muscle and tells the muscle how to behave-- super important in things like ALS, but also in aging. The slowed transmission of information across that neuromuscular junction is what causes old people to fall. Their brain cannot trigger their muscles to react fast enough.
And so we want to be able to embed these sensors to understand how these different, interconnected systems within our bodies work together. In New York, they're doing a related, but equally exciting project where they're engineering individual cells to be able to go in and identify changes in a human body. So what they'll do is-- they're calling it-- ANDREW HUBERMAN: It's wild. I mean, I love that.
I mean, this is-- I don't want to go on a tangent. But for those that want to look it up adaptive optics, there's a lot of distortion and interference when you try and look at something really small or really far away. And really smart physicists figured out, well, use the interference as part of the microscope. Make those actually lenses of the microscope.
MARK ZUCKERBERG: We should talk about imaging separately after you talk about the New York Biohub. ANDREW HUBERMAN: It's extremely clever, along those lines. It's not intuitive. But then when you hear it, it's like it makes so much sense. It's not immediately intuitive.
Make the cells that already can navigate to tissues or embed themselves in tissues be the microscope within that tissue. I love it. PRISCILLA CHAN: Totally. The way that I explain this to my friends and my family is this is Fantastic Voyage, but real life. We are going into the human body. And we're using the immune cells, which are privileged and already working to keep your body healthy, and being able to target them to examine certain things.
So you can engineer an immune cell to go in your body and look inside your coronary arteries and say, are these arteries healthy? Or are there plaques? Because plaques lead to blockage, which lead to heart attacks. And the cell can then record that information and report it back out. That's the first half of what the New York Biohub is going to do. ANDREW HUBERMAN: Fantastic. PRISCILLA CHAN: The second half is can you then engineer the cells to go do something about it.
Can I then tell a different cell, immune cell that is able to transport in your body to go in and clean that up in a targeted way? And so it's incredibly exciting. They're going to study things that are immune privilege, that your immune system normally doesn't have access to-- things like ovarian and pancreatic cancer. They'll also look at a number of neurodegenerative diseases, since the immune system doesn't presently have a ton of access into the nervous system. But it's both mind blowing and it feels like sci-fi. But science is actually in a place where if you really push a group of incredibly qualified scientists say, could you do this if given the chance, the answer is like probably.
Give us enough time, the bright team and resources. It's doable. MARK ZUCKERBERG: Yeah.
I mean, it's a 10 to 15-year project. But it's awesome, engineered cells, yeah. ANDREW HUBERMAN: I love the optimism. And the moment you said make the cell the microscope, so to speak, I was like yes, yes and yes. It just makes so much sense.
What motivated the decision to do the work of CZI in the context of existing universities as opposed to-- there's still some real estate up in Redwood City where there's a bunch of space to put biotech companies and just hiring people from all backgrounds and saying, hey, have at it and doing this stuff from scratch? I mean, it's a very interesting decision to do this in the context of an existing framework of graduate students that need to do their thesis and get a first author paper because there's a whole set of structures within academia that I think both facilitate, but also limit the progression of science. That independent investigator model that we talked about a little bit earlier, it's so core to the way science has been done. This is very different and frankly sounds far more efficient, if I'm to be completely honest.
And we'll see if I renew my NIH funding after saying that. But I think we all want the same thing. As scientists and as humans, we want to understand the way we work. And we want healthy people to persist to be healthy.
And we want sick people to get healthy. I mean, that's really ultimately the goal. It's not super complicated. It's just hard to do.
PRISCILLA CHAN: So the teams at the biohub are actually independent of the universities. ANDREW HUBERMAN: Got it. PRISCILLA CHAN: So each biohub will probably have in total maybe 50 people working on deep efforts.
However, it's an acknowledgment that not all of the best scientists who can contribute to this area are actually going to, one, want to leave a university or want to take on the full-time scope of this project. So it's the ability to partner with universities and to have the faculty at all the universities be able to contribute to the overall project, is how the biohub is structured. ANDREW HUBERMAN: Got it. MARK ZUCKERBERG: But a lot of the way that we're approaching CZI is this long-term, iterative project to figure out-- try a bunch of different things, figure out which things produce the most interesting results, and then double down on those in the next five-year push. So we just went through this period where we wrapped up the first five years of the science program. And we tried a lot of different models, all kinds of different things.
And it's not that the biohub model-- we don't think it's the best or only model. But we found that it was a really interesting way to unlock a bunch of collaboration and bring some technical resources that allow for this longer term development. And it's not something that is widely being pursued across the rest of the field. So we figured, OK, this is an interesting thing that we can help push on. But I mean, yeah, we do believe in the collaboration.
But I also think that we come at this with-- we don't think that the way that we're pursuing this is the only way to do this or the way that everyone should do it. We're pretty aware of what is the rest of the ecosystem and how we can play a unique role in it. ANDREW HUBERMAN: It feels very synergistic with the way science is already done and also fills an incredibly important niche that, frankly, wasn't filled before.
Along the lines of implementation-- so let's say your large language models combined with imaging tools reveal that a particular set of genes acting in a cluster-- I don't know-- set up an organ crash. Let's say the pancreas crashes at a particular stage of pancreatic cancer. I mean, it's still one of the most deadliest of the cancers. And there are others that you certainly wouldn't want to get.
But that's among the ones you wouldn't want to get the most. So you discover that. And then and the idea is that, OK, then AI reveals some potential drug targets that then bear out in vitro, in a dish and in a mouse model.
How is the actual implementation to drug discovery? Or maybe this target is druggable, maybe it's not. Maybe it requires some other approach-- laser ablation approach or something. We don't know.
But ultimately, is CZI going to be involved in the implementation of new therapeutics? Is that the idea? MARK ZUCKERBERG: Less so. PRISCILLA CHAN: Less so. This is where it's important to work in an ecosystem and to know your own limitations. There are groups, and startups and companies that take that and bring it to translation very effectively.
I would say the place where we have a small window into that world is actually our work with rare disease groups. We have, through our Rare As One portfolio, funded patient advocates to create rare disease organizations where patients come together and actually pool their collective experience. They build bioregistries, registries of their natural history. And they both partner with researchers to do the research about their disease and with drug developers to incentivize drug developers to focus on what they may need for their disease.
And one thing that's important to point out is that rare diseases aren't rare. There are over 7,000 rare diseases and collectively impact many, many individuals. And I think the thing that's, from a basic science perspective, the incredibly fascinating thing about rare diseases is that they're actually windows to how the body normally should work.
And so there are often mutations that when genes that when they're mutated cause very specific diseases, but that tell you how the normal biology works as well. ANDREW HUBERMAN: Got it. So you discussed basically the major goals and initiatives of the CZI for the next, say, 5 to 10 years.
And then beyond that, the targets will be explored by biotech companies. They'll grab those targets, and test them and implement them. MARK ZUCKERBERG: There's also, I think, been a couple of teams from the initial biohub that were interested in spinning out ideas into startups. So even though it's not a thing that we're going to pursue because we're a philanthropy, we want to enable the work that gets done to be able to get turned into companies and things that other people go take and run towards building ultimately therapeutics. So that's another zone.
But that's not a thing that we're going to do. ANDREW HUBERMAN: Got it. I gather you're both optimists.
Yeah? Is that part of what brought you together? Forgive me for switching to a personal question. But I love the optimism that seems to sit at the root of the CZI. PRISCILLA CHAN: I will say that we are incredibly hopeful people. But it manifests in different ways between the two of us. MARK ZUCKERBERG: Yeah. PRISCILLA CHAN: How would you describe your optimism versus mine? It's not a loaded question.
MARK ZUCKERBERG: I don't know. Huh. I mean, I think I'm more probably technologically optimistic about what can be built. And I think you, because of your focus as an actual doctor, have more of a sense of how that's going to affect actual people in their lives, whereas, for me, it's like-- I mean, a lot of my work is we touch a lot of people around the world.
And the scale is immense. And I think, for you, it's like being able to improve the lives of individuals, whether it's students at any of the schools that you've started or any of the stuff that we've supported through the education work, which isn't the goal here, or just being able to improve people's lives in that way I think is the thing that I've seen be super passionate about. I don't know. Do you agree with that characterization? I'm trying I'm trying to-- PRISCILLA CHAN: Yeah, I agree with that.
I think that's very fair. And I'm sort of giggling to myself because in day-to-day life, as life partners, our relative optimism comes through as Mark just is overly optimistic about his time management and will get engrossed in interesting ideas. MARK ZUCKERBERG: I'm late. PRISCILLA CHAN: And he's late. ANDREW HUBERMAN: Physicians are very punctual, yeah. PRISCILLA CHAN: And because he's late, I have to channel Mark is an optimist whenever I'm waiting for him.
MARK ZUCKERBERG: That's such a nice way of-- OK, I'll start using that. PRISCILLA CHAN: That's what I think when I'm in the driveway with the kids waiting for you. I'm like, Mark is an optimist. And so his optimism translates to some tardiness, whereas I'm a how is this going to happen like.
I'm going to open a spreadsheet. I'm going to start putting together a plan and pulling together all the pieces, calling people to bring something to life. MARK ZUCKERBERG: But it is one of my favorite quotes, that is optimists tend to be successful and pessimist
2023-10-24 21:48


