2021 Texas McCombs Business Outlook Series – Focus on the Future of Healthcare
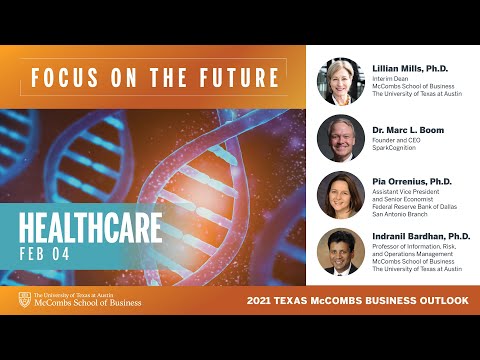
****DISCLAIMER**** THE FOLLOWING IS AN UNEDITED ROUGH DRAFT TRANSLATION FROM THE CART PROVIDER'S OUTPUT FILE. THIS TRANSCRIPT IS NOT VERBATIM AND HAS NOT BEEN PROOFREAD. THIS IS NOT A LEGAL DOCUMENT. THIS FILE MAY CONTAIN ERRORS. THIS TRANSCRIPT MAY NOT BE COPIED OR DISSEMINATED TO ANYONE UNLESS PERMISSION IS OBTAINED FROM THE HIRING PARTY. SOME INFORMATION CONTAINED HEREIN MAY BE WORK PRODUCT OF THE SPEAKERS AND/OR PRIVATE CONVERSATIONS AMONG PARTICIPANTS. HIRING PARTY ASSUMES ALL RESPONSIBILITY FOR SECURING PERMISSION FOR DISSEMINATION OF THIS TRANSCRIPT AND HOLDS HARMLESS CAPTION SOURCE FOR ANY ERRORS IN THE TRANSCRIPT AND ANY RELEASE OF INFORMATION CONTAINED HEREIN. ****DISCLAIMER**** February 4, 2021 - McCombs Business Outlook: Healthcare [ music ] >> Welcome to all our alumni, health care professionals, and students. We have 1800 registrants today. Thank you especially to McCombs alumni and all the Texas exes in attendance. This is our 9th annual collaboration between McCombs and the federal reserve bank of Dallas. We gather together and interview top economists and business executives from key industry sectors. My name is Lillian Mills. I'm from the University of Texas at Austin. All of the questions were presubmitted. We're not collecting extra ones lives. Now, between me and the three panelists, we have four doctors here, but the only medical doctor is our colleague Dr. Mark Boom. He is president and CEO of Houston Methodist, assistant professor at Cornell University, and adjunct professor in the University of Texas School of Public Health. We also welcome Dr. Pia Orrenius. She's a labor economist working on regional economic growth and demographic change and manages the regional and microeconomics group at the Dallas fed in their research department. She's also the executive editor of the quarterly Southwest Economy Publications. Then my professor colleague, Indy Bardhan, is the professor of management at UT Austin. His research focuses on health care analytics and technology. I appreciate his close collaboration with UT medical and Dell Medical School. He teaches in our new master of science health care transformation program. We've graduated our first cohort of 75 students, and the second one is underway. It's a joint program between Dell Med and McCombs where they lead value based transformations. So we're going to start talking about the COVID pandemic. Gosh, it's big, personal shockwaves around the world. More than 2 million people died globally, and that includes 34,000 people in the state of Texas. Lots of people have lost their jobs. Hospitalizations surged this winter with constrained ICU beds and opening of field hospitals. So let's start with the pandemic's economic impact in 2020, those disruptive and societal impacts, and then your expectations for health care industry and the future. Pia, if it's okay, I'm going to start with you. You've been an economist for a lot of years at the Dallas fed. The 2020 economic collapse is going to go down in the record books and be your comparison going forward. What can you tell us about big effects from the pandemic in the Texas economy, and what's your medium term outlook?
>> Thank you. It's a pleasure to be here today. The pandemic caused a recession like no other recession we've experienced. Of course, I would say it generated a fiscal and monetary response like none other either. We can come back to that later. Initially, my colleagues and I thought the pandemic was more like getting hit by a hurricane than a typical recession. We generally expected a V-shaped impact on employment and activity, which would have meant a very quick bounce back this past year. Like if you think of Houston, for example, after Hurricane Harvey, within a few months, employment was back to where it had been before the hurricane. But we should probably have listened to the epidemiologists. This is not what happened. There was a severe decline in employment and across all geographies. We lost over 11% of our employment in the state. That was over 1.4 million jobs. Just a huge impact. >> Wow. >> But then the recovery has been slower than we hoped, and a big reason is the resurgence of the virus in July and at the end of the year and what we're experiencing currently. To date, only a little over half of the jobs lost have been added back. We're down about 4.5% from where we were one year ago in terms of employment. So we really still have a ways to go. With regard to the outlook, now that the vaccine is here, our out look is positive. The Dallas fed has forecasted over 4% job growth this year, which is way above our trend rate of growth. But we still expect a first -- a slow first quarter, but then things to pick up after that. In our business out look surveys, which survey over 600 firms, most of them expect to be back to normal by the end of this year. >> Okay. So in terms of when the state of Texas is going to recoup the jobs its lost, you're thinking still in this calendar year maybe. Which sectors are going to outperform? Is which ones are lagging even in 2021? >> Yes. So even with the rapid job growth that we're predicting for this year, as I said, over 4%, we will not recover all lost jobs by the end of this calendar year. We may not -- we may be halfway through 2022 until we are back to where we started. In terms of the sector impact, the largest negative effects are on the face-to-face industries, the service sector, like hospitality and leisure, restaurants and hotels, arts and recreation venues, passenger airlines, cruises, tourism, that type of thing. Of course another problem for us in Texas has been the impact on the oil and gas sector, which has just been decimated. So they lost a quarter of jobs last year with a plunging oil prices and plunging production in the energy sector just because there was such a drop-off in demand for gasoline and jet fuel and so forth. On the other hand, some industries have been booming. So as the service sector faltered, manufacturing has hung in there. Residential construction has been just off the charts. Home sales have surged. We saw 6 percentage point increase if Texas in the homeownership rate last year which is just unprecedented. So it's a little bit tale of two cities. >> So, Marc, let's talk about the economy, but we'll move it to health care where you're stewarding a huge hospital. Seems like the health care sector has lost jobs. Why would that be true in a pandemic, and does it permanently restructure health care employment in some way?
>> I think there's a couple things to keep in mind. First, health care is a huge sector across Texas and the United States. It's diverse. It's very fragmented still in the United States and certainly in Texas. So as a result, the impact has been felt differently across different parts of the sector. You know, I'll talk about us for a second. We didn't do any layoffs. We don't do any job cuts or furloughs. When you look at those economic numbers, at the surface, you say a big hospital system didn't actually contribute to that loss of jobs overall, but if I look at our numbers, we grew far more slowly this year as we dealt with the pandemic. We're a place that would have been adding jobs. When you look at that aggregate, there's a whole bunch of diverse and kind of adding on kinds of things. Health care has this sort of reputation as being recession-proof. It is not recession-proof. It is recession-resistant. In oil and gas goes like this, we go like that at a smaller level. We still feel it. Every time, for example, oil and gas has been hit in Houston, we feel it. This spring was brutal because the craziness of how health care is funded is there's so much cross-subsidization and so much happens from the kind of elective side of things to pay for the non elective side of things. It really turned health care on its head for a couple of months. That has recovered, and you'll see that job growth coming back. Certainly right now we can't hire fast enough for the clinical people that we need. Still, the administrative side, everybody is being cautious given the challenges. So aggregate, it's slower growth. >> Let's narrow in a little further on the Affordable Care Act because one option was to take federal money to expand Medicaid coverage. The state of Texas chose not to. What effect do you think that had to access to health care during 2020 and continuing into '21?
>> There's no question we have seen a very unequal sort of response and unequal impact of COVID. So COVID in one way is the great leveler. Anybody can get it. You've seen President Trump and Boris Johnson and others. So really can affect any human on the planet. At the same time, it exposed a lot of inequities in our health system. We saw higher people in poverty, deserts in terms of food access and pharmacy access and health care coverage really be impacted in disproportionate ways. When you look at the question about Medicaid expansion, Texas is one of the states that has decided not to do that. One of the results of that is we have 18% uninsured. That's double the national rate of 9%. 39 states have now actually expanded Medicaid and addressed that. If you look back at the elections. 20 states were republican, four states were three times, three states were two times. What you're seeing is many red states have figured this out. We're a red state that hasn't. There's an ability to do this. I think it requires bipartisan action. I think if Biden is serious about bipartisan ship. That administration working with a Texas administration with others really needs to ask the question about how do we close these gaps? How do we determine at the end of the day that 18% uninsured is completely unacceptable and is going to continue to have those issues. The final thing to acknowledge is that we're going to see those numbers get much worse. We heard about the job numbers overall. Right now we haven't seen that because people still have cobra coverage by and large. That's going to flow through the economy here unless people are rehired at a rapid rate to employer sponsored health care. It's a significant issue for us. >> Thank you. Indy, let's partition a little bit. Which sectors do you think are going to have the longest term consequences of COVID-19? >> Thank you for having me on the panel. One of the things that we've observed the last about five, six years of data, health care industry as a whole has grown at a rate of about 4.7, 4.8% in that range, prior to COVID. Now, when COVID came along in March of 2020, the entire sector was hit. Hospital spending, for instance, was down about 36% just in March and April of 2020 alone. If we look at the data for the first 10 months of 2020, overall, the data shows some sectors got badly hit. Physical services was down compared to 2020, and hospital care and related services was down about 3.6%. The two sectors that have actually held steady and improved over time which we expect to do even better over time in 2021 and beyond with home health care which grew 14% last year and is expected to grow at the same rate if not more this year. Prescription drugs was about the same, about roughly 3% growth, but home health care is where a lot of the action is. This is actually borne out by the data that the two biggest areas of growth in terms of funding and other investments is telehealth and remote patient monitoring. Both of those -- both of those types of investments are actually driving the increase in home health care: Telehealth, for instance, grew from before the pandemic and only accounted between 1% and 2% of physician visits. Today it's roughly 7% of all physician visits. So it's grown by a significant factor. So in the near future, at least for 2021 and 2022, we do expect a much more evolution from a typical face-to-face model of care, outpatient care in the health care industry, to a hybrid model where you'll have some face-to-face care but also complemented by at-home care given by technologists. That's where I would expect the growth in industry. >> Thanks, Indy. I know that that's in combination with so many medical devices that can be used. I've got a relative with a diabetic under-skin monitor, and so it's not just the telehealth. It's that we've got personal devices that help facilitate the telehealth. Yeah. So an open question to any of you, if you want to answer, do you have in mind some policy initiatives that the Biden administration could implement or you wish they would implement to alleviate some of the impacts? I know, Marc, you talked about we need more bipartisan conversations, but I thought I would throw this out to anybody that had other ideas.
>> I guess economic policy, I can just start us off. I guess one of the big discussions is currently about additional stimulus, which would certainly bring the economy back sooner and faster. I guess with the current pace of vaccinations and the improvement that is already forecast for the economy without this additional stimulus, you know, there's some concern that a large stimulus program would actually overheat the economy because of the timing and the size of it. Some economists have proposed adding triggers to the stimulus which means resources would only be released if certain economic conditions were met. That's a good idea. I'm not sure if that's getting consideration by the current administration. Of course, there are other provisions that are on the table that would hurt and slow our recovery especially in Texas, something like a very large increase to the minimum waging would probably slow our jobs recovery here in this state. And, of course, I would be remiss not to mention, you know, there's a lot of discussion around regulation of oil and gas, but we've looked at it and even with these additional regulations currently, we don't think it would have a big impact on our oil and gas industry but maybe in places like New Mexico our neighboring state where they have a lot of drilling on federal land. >> Yeah. >> One of the other areas that I think I would like to mention in terms of policy that the Biden administration can do is continue with what they call the 1135 waiver for telehealth which prior to the COVID pandemic, you could only get telehealth reimbursement for very, very specific types of visits, and it was primarily aimed at the rural market. Now it's for most type of physician visits. So to continue with that waiver and expand reimbursement to incentivize virtual care would be a very important initiative for the new administration, and also just because you have telehealth doesn't mean that you've solved the issue of disparities in terms of access to underserved populations. So disparities in terms of health equity, I think more needs to be done in that area to address some of the problems where senior citizens and people who are not -- don't have access easily to, you know, digital means to access telehealth, you know, that needs to be addressed. The last item that I would mention is the ability to expand virtual health care across state lines. That would be an important factor that administration can consider.
>> Yeah. Gosh, thanks. You're right. We have some really big city centers that are near a state border. I think of you, Marc, in the Houston area. You're close to Louisiana. There could be some rural west Louisiana people that would like to have telehealth appointments with your hospital or MD Anderson. >> No question. I completely agree with all of that. This state border issue has been a real obstacle during COVID in many ways. So we need to figure that out as a health profession and the licensure side of things. >> I just wanted to add one thing that the Biden administration has before done, which is actually beneficial is -- well, they're planning to open up the ACA exchanges again for people to sign up for health insurance. So that's actually very important because as Dr. Boom was saying, cobra coverage is going to run out for unemployed workers. If they go on the exchanges and sign up for health insurance, that's a big positive.
>> Yeah. Let's turn to innovation, and I'm going to go back to you, Marc. What sort of innovations came out of the pandemic that might not have gained traction without it? I expect telehealth is one of those, but take that one and go elsewhere with it if you want. >> I think I could talk for an hour on this topic. I'll be brief because one of the silver linings is it injected steroids into the process, particularly around the digital innovation of health care especially virtual care. I would say we probably, as an industry, probably evolved five years in two months. Of the things that we were expecting to roll out we've been prepping to roll out but we recognize you've got to teach a lot of old dogs new tricks and bring your clinicians along and everything else. It happened overnight. I think that's one of the good things that happened in this pandemic. Let me give you examples. We were working on virtual ICU. So this is where we can essentially have a central command center that oversees every one of our ICU patients and beds with a trained physician with all the data there so it's not replacing the front line people. It's enhancement to that. So it brings better quality to bedside and more rapid response, et cetera. Imagine during a pandemic where you can't walk into a patient's room safely or if you do, it's a lengthy process, donning and doffing protective equipment. That has been huge and we were going to roll that out over a course of a year and turn it on and apply it to 330 ICU beds within the course of three or four weeks. With nine or ten months under our belt, this will never change. It's a huge impact. Personal touch items. We have iPads and we were rolling iPads in the rooms as a device for our patients. That's in almost every room now as an entertainment tool. We've got Alexa in about half of our patient rooms already. You can say, hey, Alexa, I need to talk to my nurse. All of those kinds of things have really been propelled forward. I'm scratching the surface of things we've done. I think that's going to be a real positive going forward. >> Boy, that's great. Sounds like you were ready for it right when it came. So you had been making those investments in advance. I've got to believe you were way ahead -- miles ahead of some rural hospitals that weren't planning for that transition. >> Yeah. You know, one of my favorite quotes is chance favors the prepared mind. It's kind of a perfect quote because this is a guy who helped found germ theory. Back in his day, he was telling the doctors to wash their hands when they wouldn't wash their hands and did early vaccine work. He's the perfect quote for that. And never has there been no true during this pandemic. So we had a center for innovation. We had virtual urgent care in place. So virtual urgent care is an example. We had about 70 of our physicians who had run towards that and were doing that and active in that. Now we have 600, 700 just in our employee base let alone all the private physicians did who do that. We were doing 3,000 visits a day at one point. If I go back a year and a half ago, we would do a couple percentage of our visits. Now 30% of our visits at a baseline, even when we're not inserted, seem to be virtual. Those things will sustain, but critically, having that preparation to talk about rural very quickly, I think this is actually one of the solution points for some of the challenges of rural health. So we're going to be partnering very actively with rural hospitals. Think of what that enables to happen in a small community? They don't have to drive 200 miles to see a specialist. Something like virtual ICU, you can pass put a mass infrastructure and enhance the quality. It's going to have positive ramifications for everybody and certainly in rural communities. >> Yeah. And Indy, pick it up from Marc and tell us some solutions.
>> Piggybacking, I agree completely. One of the positive impacts of what has happened due to the pandemic is this enhanced notion of systemness where you have greater collaboration between health systems to facilitate care for patients including between academic medical centers and community hospitals, exactly to Marc's point. And in terms of the technology, I have some numbers here, thanks to my friend local venture capitalist in Austin, Emma Cartwell. Some of her data points to funding and digital health has increased by 350% over the last five years. Just in 2020 alone, the first six months of 2020, saw about 6.3 billion in digital health investments out of which 2/3 were going towards consumer centered. Most of that investment has been in things like telehealth, about $2 million, 800 million dollars in M health companies, mobile health, clinical physician support as well as $400 million towards companies that are improving remote patient monitoring. One of the other things that has also happened and there's been some research that has shown some initial evidence that one of the things that technology has helped to enable is a fresh look at these new types of payment models for value-based care. And so our value institute and he dell medical school actually is one of the leaders and pioneers in that area in terms of implementing new payment models with respect to some of their integrated practice units. Some of the research has shown that the pandemic has had far less of a negative impact on the revenues of health systems which have -- that have implemented global payment structures. The last thing that I would like to mention in terms of technology is that many companies, for many hospitals and health systems, they have used artificial intelligence, AI analytics to improve everything from their supply chains to better and more accurate diagnosis of COVID-19 patients, for instance. Right? To accurately manage and forecast patient volume and PPE and also to optimize their resource staffing, clinical staffing. So, again, there's been a significant increase in the use of some of these new types of emerging technologies including AI and digital health investments in health care. >> Thanks, Indy. Pia, I'm going to turn to you from the perspective of your role at the fed. What investments in digital health have you been seeing from your vantage point? What's the long-term impact of those going to be? >> I'll speak more broadly to what we're seeing across all industries, not just in health care because I think Dr. Boom and Dr. Bardhan went into great detail about the health care sector. But we're generally seeing, as a result of the pandemic, a very rapid speeding up of technological innovation and technological adoption in all firms across industries. So what we're hoping comes from this is productivity increases in years to come as this technological -- Aztec knowledging really makes us more efficient and able to produce more, get better outcomes with fewer resources. So hopefully that is coming in the future which will boost growth, you know, relative to where it would have been. With that comes a challenge, and it's to the extent that technology is changing the way we do business and how we deliver care and to the extent which it's displacing workers. So when technology comes in to firm and affects operations, we may need to reconfigure, you know, the head count and who does what in a business. When that happens, to the extent people are displaced or laid off or have to, you know, go back to -- for more workforce training and so forth, we need to make sure that the resources there are for workers to retrain, to move across businesses or industries, even change occupations in response to changes in technology. I think that's the broader implication and long-run implication of what's going on. >> So I've been watching -- there is a little bit of Q&A showing up in the chat, and I'll remind you that we had 1800 registrants. We took a bunch of questions in advance of this webinar, crafted them in the best order we could, and so I'm pitching to you questions that all of you submitted earlier, but we're probably not going to be able to get to these live during this webinar. But a number of them do relate -- that I've been seeing about societal impact, and we'll turn to that in just a few minutes. So to wrap up in this economic conversation and open to any of you, if there's more you want to say about the innovations that will still be affecting us five years down the road, what is your forecast? Again, it's the silver linings is that are going to persist in the health care industry. >> I'll pick up a couple very quick thoughts. One is this has shown everybody what's possible and to do it quickly. That is one of the big silver linings. One of the things that would have taken time to implement are getting implemented quickly. We need to hold on to the gains. Even there, this is that on steroids. I think that is a big thing going forward. When you think about health care innovation, a lot of things we were both talking about, there's kind of a last mile. I think about some of the struggles sometimes, there's that last mile problem for digital health. A lot of that is then how do you get the physical exam conducted? How do you get the vital signs or listen to somebody's heart or figure out to palpate their abdomen? There's a lot that could be done if we can figure those last mile issues out. So a lot of wear able technologies and monitoring solutions and a lot of those give us that ability to care for people longitudinally. I think the opportunity for physicians and hospital systems probably as a supposed to the Silicon Valley is how to take those issues and opportunities and turn them into lifelong relationships so you can manage's somebody's care and health as opposed to just responding to their problems that they have. I think there's great opportunity. There's one of the tough problems is how do you get that last mile solution and into the patient's home or the individual's home and monitor and diagnose what you need?
>> Well, you were talking early on, Marc, about old dogs and new tricks. It occurs to me there's this huge spillover that if a generation of people who did all their banking in person with the teller, all their shopping in person at the store, all their doctoring in person at the doctor learned to shop on Amazon or Wal-Mart plus, learned to deposit checks online, the spillover to how do I trust the online telehealth, it's all re-enforcing that it's really a, do I trust the technology with all these aspects of my life and, yeah, I think those are going to have a long-term effect. >> We're seeing that people do trust them, to your point. This is -- we are a society that's been preconditioned to figure out how to trust those online. This was the year that if there was any doubt, it's gone. People do trust it. >> Yeah. Well, let's talk some about societal health around health care, and gosh, Pia, we've hinted at the idea that some people have been displaced or disproportionately affected. Do you see policies that the new federal administration is intending to or could or should implement to help the people most affected by COVID-19? >> I think in general, we have -- they have a good ear in this current administration as far as listening to people.
People have been heavily impacted and harmed by this pandemic. Although I think a lot of the policies that we need to help people along have already been put in place. So, again, we talked earlier about additional stimulus, but things around unemployment benefits are very important. Unemployment benefits, you know, continue in some form even for people that are now long-term unemployed as opposed to short-term unemployed, which is what we started out with people being short-term and that's transitioning into longer spells which is a problem. Stimulus payments came through, and I think they were very effective. We saw the consumption was really sustained especially in the low income households as a result of the generous stimulus that came across last year in the CARES Act. Now, there were certain categories of people left out of that that has been remedied. For example, certain immigrants, like undocumented immigrants, which we have a lot in Texas -- we have probably 1.5 million or so. So that stimulus has now been extended to them as well in the last round of the stimulus program. So that's helpful for them. Those families and also for the state. I think from a pandemic perspective and a public health perspective makes sense that sort of need to have everybody under one umbrella. Then there are things we mentioned earlier like workforce training, transitioning them back as the economy comes back. But then there's other things that have also been a real barrier for people that have been hurt by the pandemic. Things like child care, school closures have been a real problem. Women have been very hurt by this pandemic recession. Mostly because of problems with sending kids to school and closed child care. There is the additional issue of transportation. Transportation is sort of a long-standing issue in terms of how do we get people to the jobs that they can apply for and get hired at. So those are some issues that need to be looked into. >> Thanks, Pia. I would like to move to vaccinations and start with Indy and then flip over to Marc. So Indy, we're in the middle of rolling out vaccines. There are new shipments every week. What do you think about what we're learning about distribution mechanisms and what roll is technology playing in figuring out where to send them or how to prioritize them? It I know we're in the middle of a huge experiment with every state doing it a little bit different. So there will be research to come with a lot of semi-exogenous shocks. What are you thinking about vaccine distribution and your research? >> Thank you. I think there are several challenges, you know, with respect to the vaccine rollout. Some is of it is related to, you know, even before the rollout, associated with the manufacturing of the vaccines and there are some challenges associated with raw material constraints, the delay of production. We're talking about syringes and vials not being available. That's something that the Biden administration recently addressed. They were basically going with a 20% increase and making sure they had more availability of the vaccines at each vial. There's also quality assurance challenges in manufacturing. The third point I want to hit which is really important is some of the inequities in vaccine distribution that we see today due to the digital divide between the haves and have-nots. In terms of we're not just talking about people in different socioeconomic classes but also many elderly citizens who do not have access. You know, for instance, to make the online appointments with the local health authorities. For instance, Austin public health is our local health authority that is in charge of a lot of the vaccine rollout, and I know from firsthand experience that many of our senior citizens are having difficulty in accessing their website. They're depending on their adult kids to be able to make their appointments. So right there in terms of technology, I think a couple of things that we really would like to highlight is the role of electronic health record systems to be able to have these patients registered. So health systems can depend on electronic health records to leverage those patient registries and schedule people for the first dose and even auto schedule for the second dose. Right? And the second thing is, again, the role of mobile health technologies, auto notification of our patients especially in underserved communities. For instance, one of the popular telehealth platforms, they have partnered with the city of Chicago to actually use the telehealth platform to reach out to minority communities to schedule their vaccination appointments. So, again, there's a whole role of AI, again, in this -- in terms of how to make this process a lot more smoother, but I think I'm going to stop here due to the time constraints. >> And, Marc, do you have anything on the ground from Houston about vaccination, either related to your hospital or just what you're seeing in your city that you wanted to share? >> Yeah. I agree with everything that was just said. The fundamental challenge we have right now -- and there's many things. Don't get me wrong. There's not enough vaccine. That's the number one constraint that is occurring right now. So I'll give you our experience. We've done 133,000 vaccinations as of yesterday. 95,000 are first patients. Next day or so, we'll pass 100,000 individuals vaccinated. We get it into people's arms the week it comes. We could be doing twice as much to three times as much each and every week. We're only one of the channels in Houston and we have not tapped all the other channels. We've done a collaborative plan across the Texas medical center institutions with the county, with the city and looked at, if he we wanted to herd immunize, it's 7.1 million people. Kids aren't eligible yet. It's 5.5 million eligible individuals, which actually to get to herd immunity, we need to vaccinate almost every adult. That is basically about 52,000 shots a day that need to be administered in the city -- in the greater Houston area for six months and you'll get to herd immunity in six months. We're getting first shots. That number I gave you of 52 is both shots. We're getting 65,000 a week on average right now into the city. So we need somewhere around 175,000 first shots alone coming in a week. So we're getting less than half of the supply to get there. So the biggest challenge is still that. Many other challenges in terms of scheduling. I can re-enforce those inequity issues, the digital divide issues, different uptake rates, different vaccine hesitance and skepticism across different groups of people. Those are real dramatic significant challenges. We've probably even seen the "New York Times" report. Even when you target into a vulnerable zip code, you find that you have disparities happen in that zip code because of the digital divide, because of different groups of people having different kinds of access. So it is a real challenge that everybody is on the ground working on.
>> So I look at that as being part of the public health ecosystem or crisis. What do you see for the next two to five years? Do you have any hope you can give us about public health or concerns that we just need to keep looking at even when this pandemic has passed? Anybody that wants to, talk to us about the public health landscape in the next five years. >> I think we're -- go ahead. >> Please, go ahead, Pia. >> Well, I'll just speak generally and then you can speak more specifically. Just in general, our health care system just obviously has a lot of problems. We spend in this country over 18% of our GDP on health care and we get worse outcomes than nations that spend a lot less. So we have a lot of changes that we need to make. I think we're learning, but we're learning slowly how to address those changes that need to be made. I think Affordable Care Act was designed by an economist. I guess I'm bias. But he had some ideas about some of the changes that need to be made in order to improve health care delivery and outcomes. So I'll just -- I think there's lots of -- there's so many problems in the health care system that in the United States that we, I guess the good news is there is that there's a lot we can do. It's not like a problem that's insurmountable. There are things we can do to improve it. Hopefully the pandemic will speed the changes up and increase thingness to undertake those changes. >> Yeah. I think if there's one thing the pandemic has shown us is that we have dramatically underinvested in public health. So whether you're talking at the federal level, the state level, the local county level, city level, we're not investing enough. We have not put in place from a pandemic preparedness standpoint anywhere remotely near the investments we could be putting in to prevent the situation we're in today. I think it will pay significant dividends. If you look at actually the last century, the things that actually changed life expectancy the most were public health. It was potable water and vaccines. We're arguing about whether they are the right thing to do when they are clearly the right thing to do from a public health standpoint. We got caught flat-footed. It's not just the U.S. It's the entire world because we're not investing in public health. We know they have had to respect. >> One other thing I would like to add is just there's going to be a greater focus on mental and behavior health issues. Telehealth is great, but there's going to be a significant greater focus on mental and behavioral health issues. The last thing would be, I would say, use of more systems engineer type concepts and principles with prove the efficiency of our health system.
>> I know here on college campuses and UT specifically, we care a lot about mental and behavioral health with our students. So much so that the individual colleges themselves now have mental health counseling resources embedded in each of the colleges. UT is not alone in seeing a real increase in the needs and appointments and the severity of concerns that students have trying to go to college when their families have financial distress or health difficulties. So it's a tough year, and I'm glad we've got more ways to reach people in this tough year. Does anyone want to try a political forecast? We have a fairly split, you know -- the democrats have the tie breaking vote in the senate. What's your prediction of the likelihood of some sort of Medicare for all or a big expansion of public health availability in our current administration? >> It's not going to be me, guys. [ LAUGHTER ] >> I'll jump in. First of all, Medicare for all is a horrible idea. Let me just start with that. It's not the solution to the issues. Biden has come out and said the answer -- he said this all along. The answer is to build on an infrastructure that's been in place now for 7 years since it actually got implemented over a decade since it got passed. Like it or dislike it, I think it's hard to argue with the fact that we've seen significant decrease in uninsured rates that has gone forward with it. Once rates and things stabilized, it's been stable the last few years. So Medicare for all, I honestly -- you can tell my opinion on this, but it's mediocrity for all. When you look at how it's financed, you're going to up end the system. They are getting something they think is good right now because everybody else is paying for it. If you move everybody to Medicare, you don't have everybody else paying for it and you're not going to get the same thing. That gets down to the questions of value-based health and population health and investments in public health and alignment of incentives and all those things that can happen going forward. So I don't think we're going to see Medicare for all. I don't think that's what Biden said he wants to do. From what I've seen so far, most of his priorities are non-health care. That's another thing to remember. When he talked about his key priorities, you don't see health care access on there. Part because I think he's seen how -- what a political land mine that is every time someone goes through it. So he's talking about, you know, many other things other than health care. >> Okay. Well, I wish we could ask even more questions. I'm looking at the time and so I'm going to wrap us up. Thank you, Marc and Indy and Pia for all of your insights. I'm coming away optimistic that this urgency of innovation, that spirit can stay with us not only in the health care industry but elsewhere. I hope you can all join us on February 11th where we will focus on technology and innovation. Thank you to all of you that tuned in, and hook 'em horns.
****DISCLAIMER**** THE PRECEDING IS AN UNEDITED ROUGH DRAFT TRANSLATION FROM THE CART PROVIDER'S OUTPUT FILE. THIS TRANSCRIPT IS NOT VERBATIM AND HAS NOT BEEN PROOFREAD. THIS IS NOT A LEGAL DOCUMENT. THIS FILE MAY CONTAIN ERRORS. THIS TRANSCRIPT MAY NOT BE COPIED OR DISSEMINATED TO ANYONE UNLESS PERMISSION IS OBTAINED FROM THE HIRING PARTY. SOME INFORMATION CONTAINED HEREIN MAY BE WORK PRODUCT OF THE SPEAKERS AND/OR PRIVATE CONVERSATIONS AMONG PARTICIPANTS. HIRING PARTY ASSUMES ALL RESPONSIBILITY FOR SECURING PERMISSION FOR DISSEMINATION OF THIS TRANSCRIPT AND HOLDS HARMLESS CAPTION SOURCE FOR ANY ERRORS IN THE TRANSCRIPT AND ANY RELEASE OF INFORMATION CONTAINED HEREIN.
2021-02-26 05:14


